Summary
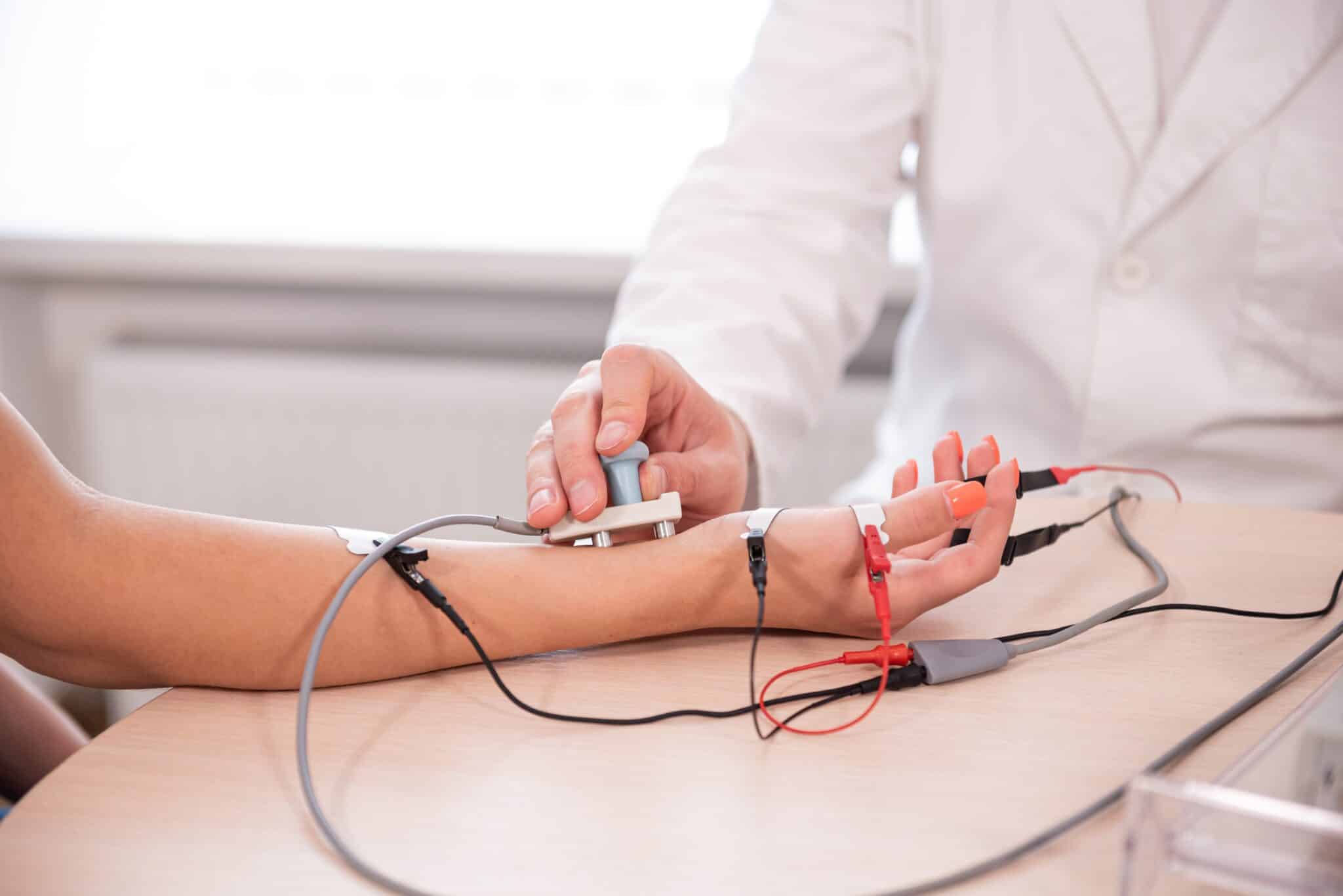
Electromyography (EMG) and Nerve Conduction Study (NCS) are non-invasive diagnostic procedures that help doctors evaluate the health and function of your muscles and nerves. If you’re experiencing symptoms like pain, numbness, tingling, or weakness, your doctor may recommend an EMG and NCS to help diagnose and evaluate nerve-related conditions. The tests involve the use of electrodes that are placed on the skin or inserted into the muscle to measure the electrical signals generated by nerve and muscle fibers during contraction and when at rest.
The procedure takes about 30 minutes to an hour and is used to diagnose muscle disorders, nerve injuries, and certain neurological disorders of the peripheral nervous system.
What is an electromyography (EMG)?
An electromyography (EMG) is a diagnostic procedure used to evaluate the electrical activity of muscles and the corresponding nerve signals that control them. It provides valuable information about the health and functioning of your muscles and nerves.
During an EMG, a fine needle, called an electrode, is inserted into specific muscles in the area that is being examined. These electrodes detect and record the electrical signals generated by your muscles when they contract or relax. The recorded signals are displayed on a monitor for further analysis.
What is a Nerve Conduction Study (NCS)?
A nerve conduction study (NCS) is a medical test used to assess the health and functioning of the peripheral nervous system, which includes the nerves outside the brain and spinal cord. It is a diagnostic procedure that helps in evaluating nerve damage or detect nerve-related disorders, and can determine the extent and location of nerve injuries or abnormalities.
During a nerve conduction study, small electrical currents are applied to specific nerves using surface electrodes placed on the skin. These electrical impulses stimulate the nerves, and the resulting responses are recorded and analyzed.
Nerve conduction studies are often used to diagnose and evaluate conditions affecting the peripheral nervous system, such as peripheral neuropathy, carpal tunnel syndrome, radiculopathy, and other nerve injuries or disorders. The test is generally safe and non-invasive, although it may cause mild discomfort or a sensation similar to a small electric shock during the procedure.
When are EMG and NCS Used?
Electromyography (EMG) is most often performed in conjunction with Nerve Conduction Studies (NCS), which together can provide valuable insight into the functioning of our neuromuscular and peripheral nervous system and help diagnose various conditions. Below are various conditions that EMG and NCS can help diagnose.
Radiculopathy
Radiculopathy refers to the compression or irritation of nerve roots as they exit the spinal cord in the spine. Sciatica, for example, is a type of radiculopathy. NCS and EMG can help determine the level and severity of the nerve root involvement and differentiate between different levels of radiculopathy.
Nerve Entrapment and Compression Syndromes
NCS and EMG are valuable tools in identifying nerve entrapment or compression syndromes, which commonly occur in conditions like carpal tunnel syndrome and cubital tunnel syndrome. These conditions involve the compression or entrapment of nerves, leading to symptoms like pain, numbness, tingling, and weakness. By pinpointing the affected nerves and assessing the severity of the condition, NCS and EMG are extremely important in determining an appropriate treatment plan.
Nerve Injuries
NCS plays a crucial role in evaluating nerve injuries, such as those resulting from trauma, surgery, or other causes. It helps in localizing the site of injury, assessing the extent of nerve damage, and monitoring the recovery progress over time.
Neuromuscular Disorders
NCS and EMG are invaluable tools used to assist in diagnosing neuromuscular junction disorders like myasthenia gravis and other muscle disorders, such as myopathies, amyotrophic lateral sclerosis (ALS) and muscular dystrophies. They provide information about nerve-to-muscle communication and the electrical activity within the muscles by analyzing the electrical signals produced by muscles.
Pre-surgical Assessment
NCS and EMG may be conducted before certain surgical procedures, especially those involving nerves or the neuromuscular system. It helps in identifying any pre-existing nerve abnormalities, determining baseline nerve function, and assisting in surgical planning.
What to Expect During the Test
If your healthcare provider has recommended a Nerve Conduction Study (NCS) or electromyography (EMG), it’s natural to have questions and concerns about what to expect. Most often, NCS and EMG are performed together during the same visit. We’ll discuss the typical steps involved below.
Preparing for the NCS and EMG
Before the procedure, your healthcare provider will provide specific instructions to ensure a successful test. These may include avoiding lotions or creams on your skin, discussing any medications you are taking, and informing them of any bleeding disorders or implanted medical devices.
The NCS Procedure
- Preparation: You will be asked to lie down or sit in a comfortable position. The area to be tested will be exposed, such as your arm, leg, or another specific body part. The technician or doctor will attach surface electrodes (small adhesive patches) to your skin at specific points along the nerve pathway being evaluated. These electrodes will send and receive electrical signals.
- Stimulation: The provider will use a handheld device to deliver a small electrical impulse to the nerve being examined. You may feel a mild, brief tingling sensation or a twitch in the muscle associated with the stimulated nerve. While the sensation might be slightly uncomfortable, it is usually tolerable.
- Recording: Other electrodes placed along the nerve pathway will record the electrical responses generated by the stimulated nerve. The provider may need to move the electrodes along the pathway to test different segments of the nerve.
- Post Test: After the NCS, you can resume your normal activities without any restrictions. There is typically no recovery period or downtime required.
The EMG Procedure
- Placement of Electrodes: During the EMG test, the healthcare provider will use a needle electrode, a fine sterile needle, and insert it into targeted muscles, one muscle at a time. You may experience slight discomfort during needle insertion, similar to a quick pinprick. The number of muscles tested depends on the condition being evaluated.
- Muscle Activity Assessment: Once the electrode needle is in place, the healthcare professional will ask you to relax or contract specific muscles. As you do so, the EMG machine will detect and record the electrical signals generated by your muscles. This process helps evaluate muscle activity and detect any abnormalities.
- Completion of the Test: Once the required data is collected from the muscles and nerves being examined, the needle electrode will be removed. There is typically no recovery period or downtime required.
How long does the study take?
The length of the NCS and EMG procedures vary depending on the area being tested. It can last anywhere from 30 minutes to an hour.
Does it hurt?
While some individuals may find certain aspects of the test mildly uncomfortable, such as the insertion of needles or the brief electrical impulses, the discomfort is generally minimal and temporary.
Who should avoid NCS and EMG?
In general, Nerve Conduction Study (NCS) and Electromyography (EMG) are safe procedures that can provide valuable diagnostic information. However, there are certain situations where caution or avoidance may be necessary.
- Bleeding Disorders: If you have a bleeding disorder or are taking blood-thinning medications (such as warfarin), your healthcare provider may need to evaluate the risks versus benefits of the EMG portion of the test. They may suggest alternative testing methods or adjust your medication regimen prior to the procedure to minimize bleeding risks.
- Skin Infections: If you have an active skin infection or an open wound in the area where the NCS electrodes or EMG needle would be placed, it may be necessary to postpone the test until the infection has resolved. Performing the procedure in such circumstances could potentially worsen the infection or introduce bacteria into the deeper tissues.
- Implanted Devices: If you have certain types of implanted devices such as pacemakers, defibrillators, or deep brain stimulators, special precautions may need to be taken. NCS involves the use of electrical signals, which can potentially interfere with the functioning of these devices. Your healthcare provider will coordinate with the appropriate specialists to determine if an NCS is safe or if alternative diagnostic methods should be considered.
- Pregnancy: Although NCS and EMG are generally safe during pregnancy, it is recommended to discuss the potential risks and benefits with your healthcare provider. They can provide guidance based on your specific situation and determine if any modifications or precautions are necessary.
Final Thoughts
Overall, NCS and EMG are valuable tools that provide important information for diagnosing and managing various conditions affecting muscles and nerves. By understanding the procedure and potential considerations, we hope you feel more informed and prepared when undergoing this diagnostic procedure.