What is a vertebroplasty?
Vertebroplasty is a minimally invasive surgical procedure used to treat spinal compression fractures. It involves injecting a type of bone cement into the fractured vertebrae to stabilize and strengthen the bone.
What is a compression fracture?
Compression fractures of the spine occur when one or more vertebrae (bones of the spine) become compressed or collapsed. This can cause pain, reduced mobility, and other symptoms.
The most common cause of compression fractures of the spine is osteoporosis, a condition that weakens bones and makes them more prone to fractures. Other causes include trauma to the spine, such as from a fall or car accident, and cancer that has spread to the bones of the spine.
When is a vertebroplasty used?
Vertebroplasty is a minimally invasive procedure that is used to treat compression fractures of the spine, particularly those caused by osteoporosis. It is typically recommended when other conservative treatments, such as pain medications and bracing, have failed to provide adequate relief.
Some of the specific indications for using vertebroplasty to treat a compression fracture include:
- Severe pain: Patients with compression fractures of the spine may experience severe pain that does not respond to other treatments.
- Limited mobility: Compression fractures can also lead to a reduction in mobility and may limit the ability to perform daily activities.
- Presence of osteoporosis: Patients with osteoporosis, a condition that weakens bones, are at higher risk of developing compression fractures of the spine.
- Recent fracture: If a compression fracture of the spine is recent, vertebroplasty may be recommended to prevent further damage and reduce the risk of complications.
- Fracture in a weight-bearing area: If the compression fracture is located in a weight-bearing area of the spine, such as the lumbar region, vertebroplasty may be recommended to prevent further damage and improve mobility.
What is the difference between a vertebroplasty and a kyphoplasty?
Vertebroplasty and kyphoplasty are both minimally invasive procedures used to treat compression fractures of the spine, but there are some differences between the two procedures.
Vertebroplasty
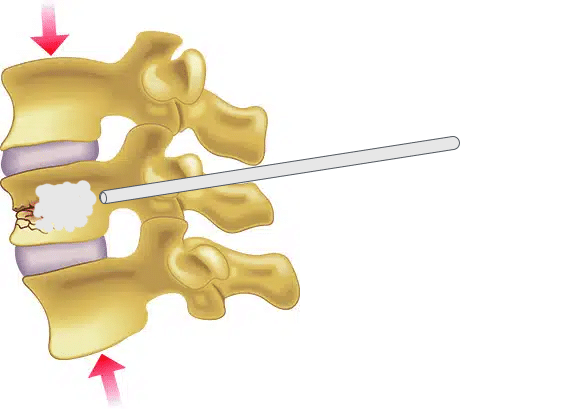
Vertebroplasty involves the injection of a special cement-like material directly into the fractured vertebra to stabilize it and provide pain relief. During the procedure, a small needle is inserted into the vertebra and the cement-like material is injected. Vertebroplasty does not involve the use of a balloon or any other tools to restore the height of the vertebra.
Kyphoplasty
Kyphoplasty is similar to vertebroplasty, but it involves the use of a small balloon to create a space in the fractured vertebra before the cement-like material is injected. The balloon is inserted into the vertebra and inflated, which helps to restore the height of the vertebra and create a cavity for the cement-like material. The balloon is then removed and the cement-like material is injected into the cavity.
One advantage of kyphoplasty over vertebroplasty is that it may help to restore the height of the compressed vertebra, which can improve spinal alignment and reduce the risk of developing a spinal deformity such as kyphosis (a forward curvature of the spine).

What can be expected during the procedure?
The procedure generally takes about 1-2 hours to complete and typically involves the following steps:
- Patient positioning: The patient lies face down on an X-ray table with a cushion placed under the abdomen to help push the spine upward and create space between the vertebrae.
- Needle insertion: The skin over the area where the fracture is located is numbed with a local anesthetic. A small needle is then inserted through the skin and muscle and into the fractured vertebra.
- Cement injection: Once the needle is in place, a special cement-like material is injected into the fractured vertebra under X-ray guidance. The cement material is injected slowly to minimize the risk of leakage or other complications.
- Repeat injection: The needle may be repositioned and additional cement material may be injected into the vertebra to fill any remaining spaces and ensure that the vertebra is adequately stabilized.
- Post-procedure monitoring: After the procedure, the patient is monitored for a short time to ensure that there are no immediate complications. Most patients are able to go home the same day and can resume normal activities within a few days.
What is the recovery time after a vertebroplasty?
Most patients are able to resume normal activities within a few days following the procedure however recovery time after can vary depending on the individual patient and the extent of the procedure.
Patients may be advised to rest and limit activity for the first 24-48 hours after the procedure and avoid strenuous activity, heavy lifting, or bending at the waist for at least several weeks after the procedure.
What are the risks of vertebroplasty?
As with any medical procedure, vertebroplasty carries some risks and potential complications. Some of the risks of vertebroplasty include:
- Infection: There is a risk of infection at the injection site or in the surrounding tissues.
- Bleeding: There is a small risk of bleeding during or after the procedure, particularly if the patient is taking blood-thinning medications.
- Nerve damage: There is a risk of nerve damage during the procedure, which could result in pain, numbness, or weakness in the affected area.
- Cement leakage: There is a risk that the cement-like material used to stabilize the vertebra could leak into surrounding tissues, which could cause pain or other complications.
- Allergic reaction: Some patients may have an allergic reaction to the materials used during the procedure.
Is vertebroplasty right for me?
Whether or not vertebroplasty is the right treatment option for you will depend on a variety of factors, including the severity and location of your compression fracture, your overall health, and your preferences and goals for treatment. It is important to discuss your options with a qualified healthcare provider who can evaluate your individual case and recommend the most appropriate treatment plan for you.