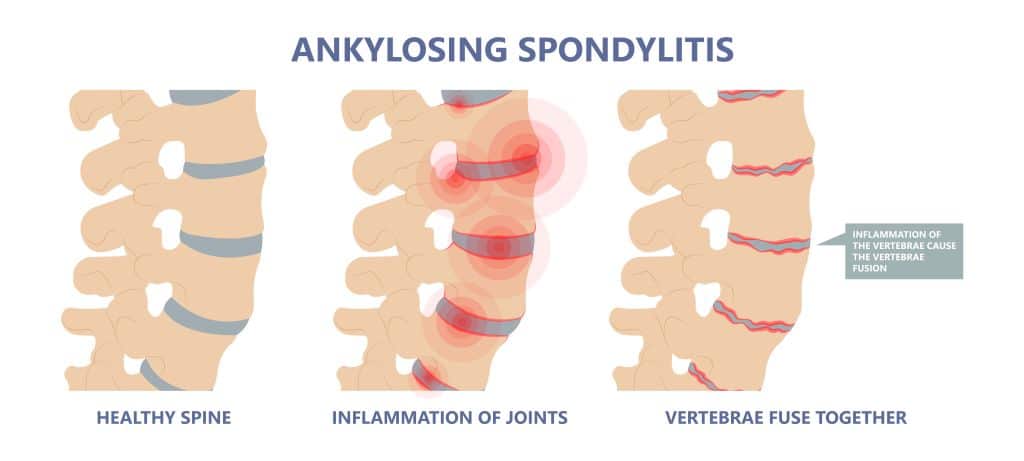
Ankylosing spondylitis is a type of autoimmune arthritis that primarily affects the spine. It causes inflammation in the joints between the vertebrae, as well as in the joints between the spine and the pelvis. This inflammation can lead to the fusion of the affected joints, causing the spine to become stiff and inflexible. Diagnosis is often made with imaging studies and lab tests. Treatment typically includes anti-inflammatory medications and physical therapy.
What is Ankylosing Spondylitis?
Ankylosing spondylitis is a type of inflammatory arthritis that primarily affects the spine and the joints between the spine and pelvis (called the sacroiliac joints). It is believed to be an autoimmune disease, which means that the immune system mistakenly attacks healthy tissues in the body. The chronic inflammation can cause the spine to become fused, or “ankylosed”.
Causes of Ankylosing Spondylitis
The exact cause of ankylosing spondylitis is unknown. It is believed to be related to genetics and the immune system.
Research suggests that ankylosing spondylitis is an autoimmune disease, a condition in which the immune system that mistakenly attacks healthy cells and tissues in the body. This can lead to inflammation in the joints and other tissues, causing the symptoms of the condition.
Ankylosing spondylitis is associated with a gene called HLA-B27, which is present in about 8 out of 10 people with the condition. However, not everyone with the gene develops ankylosing spondylitis, and not everyone with ankylosing spondylitis has the gene. This suggests that other factors, such as environmental triggers, may also play a role in the development of the condition.
Prevalence
According to the World Health Organization, the overall prevalence of ankylosing spondylitis is estimated to be 0.1-1% of the global population. However, the prevalence of the condition may be higher in certain populations, such as people of Northern European descent and those of African ancestry.
In the United States, the prevalence of ankylosing spondylitis is estimated to be around 0.5-1.4% of the population. The condition is more common in men than in women, with a male-to-female ratio of approximately 3:1.
It is important to note that the prevalence of ankylosing spondylitis may be underestimated, as the condition is often underdiagnosed or misdiagnosed due to its varied and sometimes subtle symptoms.
Symptoms of Ankylosing Spondylitis
The symptoms of ankylosing spondylitis vary from person to person and may range from mild to severe. The most common symptoms of ankylosing spondylitis include:
- Back pain: This is usually the first symptom of ankylosing spondylitis and is often worse in the morning or after periods of inactivity.
- Stiffness: The stiffness is often worst in the morning and may improve with movement.
- Other joint pain: Ankylosing spondylitis can also affect other joints in the body, such as the hips, knees, and shoulders, causing pain and stiffness in these areas.
- Inflammation of the eyes: Ankylosing spondylitis can cause inflammation of the eye called iritis or uveitis, which can cause redness, pain, and sensitivity to light.
- Abnormal posture: In severe cases, the spine may become fused or “ankylosed,” leading to an abnormal posture.
Diagnosing Ankylosing Spondylitis
There is no single test that can definitively diagnose ankylosing spondylitis, so the diagnosis is often made based on a combination of clinical examination, blood tests, and x-ray.
History and Physical Examination
Your doctor will ask about your symptoms and medical history, including any family history of ankylosing spondylitis or other forms of spondyloarthritis. They will perform a physical examination to check for signs of inflammation and stiffness in the spine and other joints.
Laboratory Tests
Some blood tests that may be used to diagnose ankylosing spondylitis include:
- Erythrocyte sedimentation rate (ESR): This test measures the rate at which red blood cells settle to the bottom of a tube. A high ESR may indicate the presence of inflammation in the body.
- C-reactive protein (CRP): This test measures the level of CRP, a protein that is produced by the liver in response to inflammation. A high CRP level may indicate the presence of inflammation.
- Rheumatoid factor (RF): This test measures the level of RF in the blood. RF is an antibody that is produced in response to inflammation and is often found in people with autoimmune conditions, such as rheumatoid arthritis. A positive RF test may be seen in people with ankylosing spondylitis, although it is not specific to this condition.
- HLA-B27: This test is used to detect the presence of the HLA-B27 gene, which is found in a high percentage of people with ankylosing spondylitis. However, a positive HLA-B27 test does not definitively diagnose ankylosing spondylitis and must be interpreted in the context of other diagnostic tests and clinical findings.
Imaging: X-rays
X-rays of the spine may be taken to look for changes in the bones that are characteristic of ankylosing spondylitis. Some of these findings include:
- Syndesmophytes: These are bony bridges that form between the vertebrae (bones of the spine). They are caused by chronic inflammation and may lead to a loss of mobility and an abnormal posture.
- Ankylosis: This is the complete fusion of the vertebrae, resulting in a loss of mobility and an abnormal posture. Ankylosis is more likely to occur in the lumbar (lower) spine and may be accompanied by the development of syndesmophytes.
It is important to note that the diagnosis of ankylosing spondylitis can be difficult and may require multiple visits to the doctor and a combination of different diagnostic tests.
Treatment of Ankylosing Spondylitis
There is no cure for ankylosing spondylitis, but it can be managed with medications, physical therapy, and other treatments.
Treatment for ankylosing spondylitis typically involves a combination of the following approaches:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help to reduce inflammation and pain. Other medications, such as disease-modifying antirheumatic drugs (DMARDs) or biologic agents, may be used to slow the progression of the disease and improve symptoms. More information on the medications to treat ankylosing spondylitis can be found below.
- Physical therapy: Physical therapy can help to improve flexibility, strength, and range of motion in the spine and other affected joints. Techniques such as stretching and exercises can help to maintain or improve mobility.
- Surgery: In some cases, surgery may be needed to repair or stabilize damaged joints or to correct abnormalities in the spine.
Medications
Some medications that may be used to treat ankylosing spondylitis include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as ibuprofen or naproxen, can help to reduce inflammation and pain. These medications are often the first line of treatment for ankylosing spondylitis.
- Disease-modifying antirheumatic drugs (DMARDs): DMARDs, such as methotrexate or sulfasalazine, work by modifying the immune system’s response to inflammation. They do this by inhibiting the production of certain proteins that are involved in the immune response or by altering the activity of immune cells. These medications are typically used in people with more severe ankylosing spondylitis.
- Biologic agents: Biologic agents are medications made using living cells. They work by targeting specific proteins or cells in the immune system that are involved in the inflammatory process. Tumor necrosis factor (TNF) inhibitors, such as etanercept and adalimumab, work by inhibiting the production of TNF, a protein that is involved in the immune response. Another class is the Interleukin-17 (IL-17) inhibitors, such as Secukinumab and Ixekizumab, which inhibit the pro-inflammatory cytokine known as IL-17.
It is important to work closely with a healthcare team to develop a treatment plan that is tailored to your specific needs and goals. Treatment for ankylosing spondylitis may need to be adjusted over time as the condition progresses and your symptoms change.
Prognosis
The prognosis for ankylosing spondylitis varies from person to person and depends on a number of factors, including the severity of the condition, the effectiveness of treatment, and the individual’s overall health.
In general, the prognosis for ankylosing spondylitis has improved in recent years due to advances in treatment. With appropriate management, many people with ankylosing spondylitis are able to maintain good quality of life and can continue to work and participate in physical activities.
Sources
Dean, Linda E et al. “Global prevalence of ankylosing spondylitis.” Rheumatology (Oxford, England) vol. 53,4 (2014): 650-7. doi:10.1093/rheumatology/ket387
Wenker KJ, Quint JM. Ankylosing Spondylitis. [Updated 2022 Apr 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470173/
Clegg, Daniel O. “Treatment of ankylosing spondylitis.” The Journal of rheumatology. Supplement vol. 78 (2006): 24-31.