Rheumatoid arthritis (RA) is a type of autoimmune disorder that causes inflammation in the joints and surrounding tissue. In people with RA, the immune system mistakenly attacks the tissues in the joints, causing inflammation and damage. This can lead to symptoms such as joint pain, stiffness, swelling, and loss of function. Treatment for RA typically involves a combination of medications and lifestyle changes to manage the inflammation and pain, and to help prevent joint damage.
What is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a type of autoimmune disorder that causes inflammation in the joints and surrounding tissue. It is a chronic (long-term) condition that can affect people of all ages, but it most commonly develops in middle-aged or older adults. It typically affects the smaller joints in the hands and feet, but it can also affect the wrists, elbows, shoulders, hips, knees, ankles and spine.
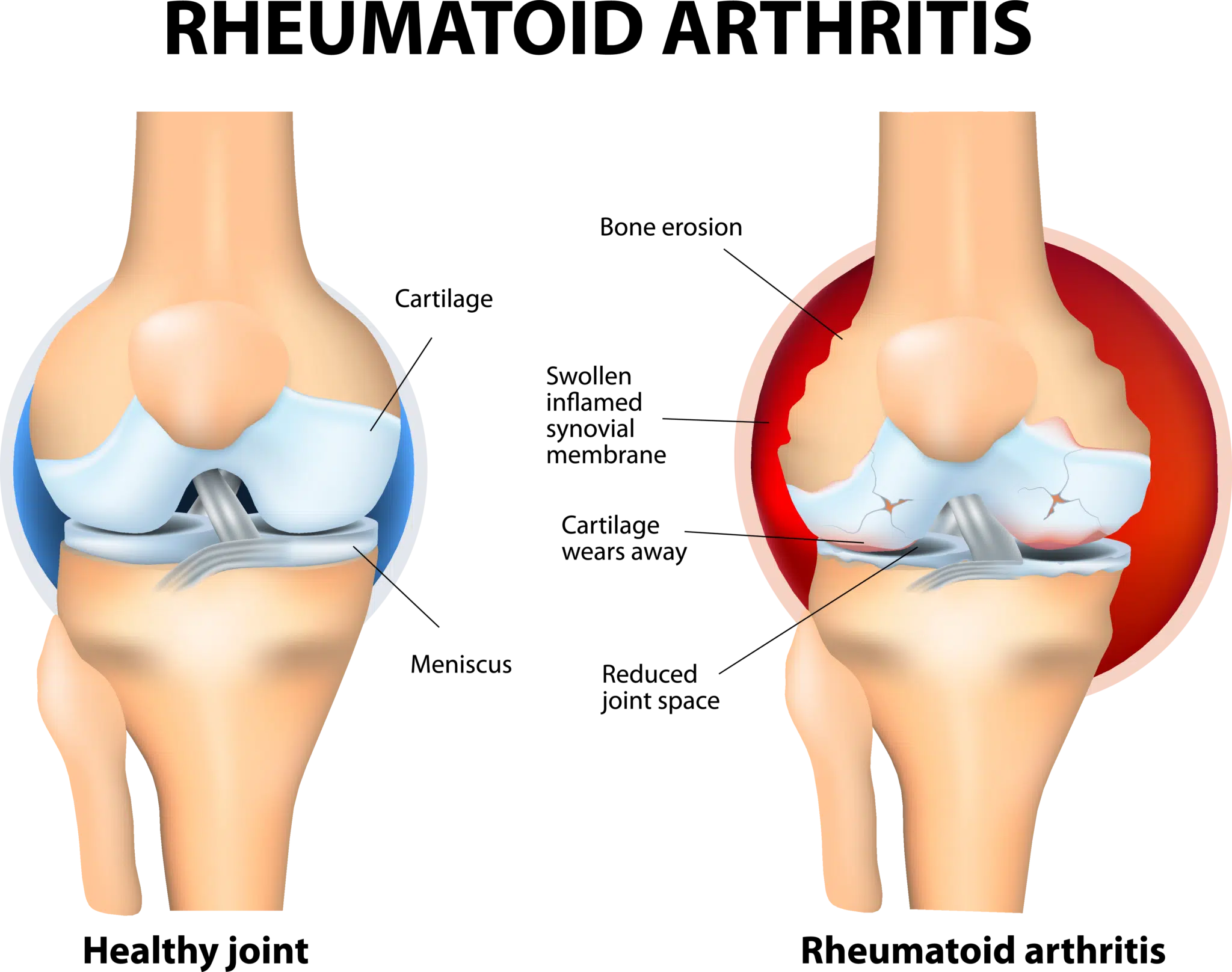
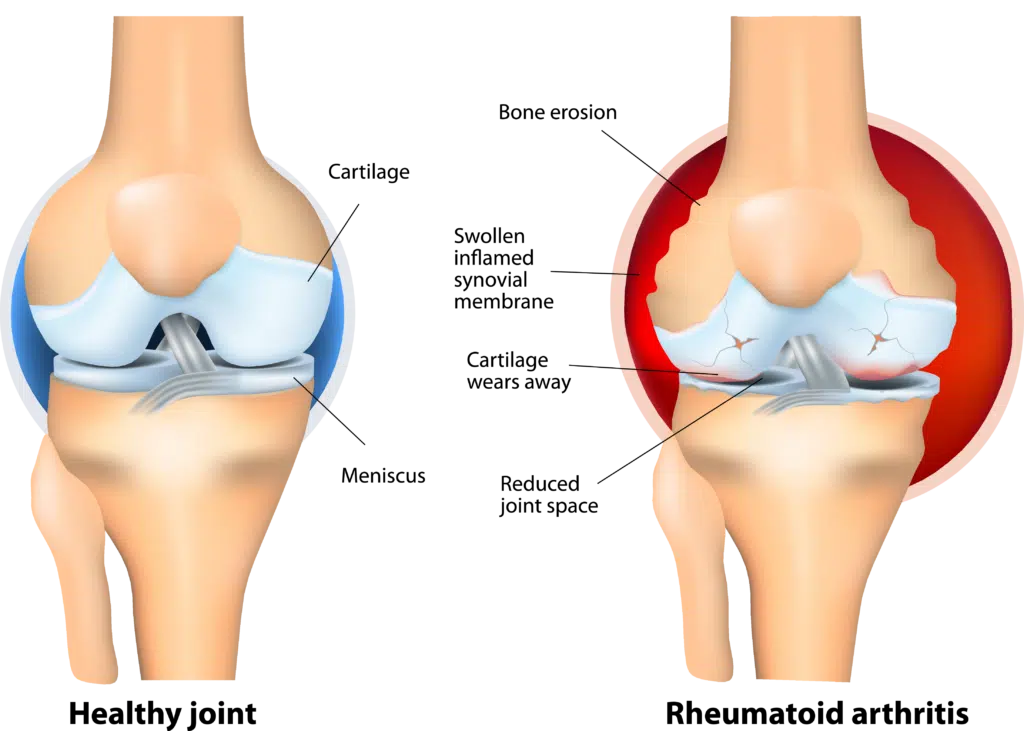
In people with RA, the immune system mistakenly attacks the tissues in the joints, causing inflammation and damage. This can lead to symptoms such as joint pain, stiffness, swelling, and loss of function. RA can also affect other organs in the body, such as the skin, eyes, and lungs.
Causes of Rheumatoid Arthritis
The exact cause of rheumatoid arthritis (RA) is not fully understood, but it is believed to be a combination of genetic and environmental factors. RA is an autoimmune disease, which means that the immune system mistakenly attacks healthy cells in the body. In the case of RA, the immune system attacks the lining of the joints (called the synovium), leading to inflammation and damage to the joint tissue. This can result in pain, swelling, and difficulty moving the joint.
There are several factors that may increase the risk of developing RA, including:
- Family history: People with a family history of RA are more likely to develop the disease.
- Smoking: Smoking is a known risk factor for RA.
- Age: RA is most common in people between the ages of 40 and 60, although it can occur at any age.
- Gender: RA is more common in women than in men.
- Environmental factors: Certain environmental factors, such as exposure to certain infections or toxins, may increase the risk of developing RA.
It is important to note that having one or more of these risk factors does not mean that a person will definitely develop RA. Similarly, not having any of these risk factors does not guarantee that a person will not develop the disease.
Prevalence
Rheumatoid arthritis affects approximately 0.5% of the global population. The prevalence of RA is also higher in women than in men, with some estimates suggesting that women are 2 to 3 times more likely to develop RA than men.
It is typically more common in people between the ages of 40 and 60, although it can occur at any age.
Symptoms of Rheumatoid Arthritis
The symptoms of rheumatoid arthritis (RA) can vary from person to person, but common symptoms include:
- Joint pain, swelling, and stiffness: RA typically affects the smaller joints in the hands and feet, although it can other joints including the spine. The affected joints may be painful, swollen, and stiff, particularly in the morning or after periods of inactivity.
- Fatigue: Many people with RA experience fatigue, which can be caused by the inflammation and the body’s efforts to fight it.
- Fever: Some people with RA may experience low-grade fever, especially during periods of active disease.
- Dry mouth and dry eyes: RA can cause inflammation in the salivary glands and tear glands, which can lead to dry mouth and dry eyes.
- Nodules: Some people with RA may develop nodules, which are small, firm lumps that form under the skin, typically around the joints.
Rheumatoid Arthritis and the Spine
Rheumatoid arthritis (RA) can affect the spine in several ways. It can cause inflammation and damage to the joints between the vertebrae (called the facet joints), as well as the bones and ligaments of the spine. This can lead to back pain, stiffness, and difficulty moving the spine.
RA can also cause inflammation and damage to the sacroiliac joints, which are located at the base of the spine where the pelvis meets the spine. This can cause pain in the lower back or buttocks.
Diagnosis
Rheumatoid arthritis (RA) is typically diagnosed by a healthcare provider based on a combination of factors, including history and physical examination, lab tests, and in some cases, imaging.
History and Physical Examination
Your doctor will ask about your symptoms and past medical history. They will ask about a family history of rheumatoid arthritis or other autoimmune disorders. They will perform a physical examination to check for signs of inflammation, swelling, and stiffness in your joints.
Laboratory Tests
There are several blood tests that may be used to help diagnose rheumatoid arthritis (RA) and rule out other conditions. These tests may include:
- Rheumatoid factor (RF) test: RF is an antibody that is often present in people with RA. A positive RF test result may indicate the presence of RA, although a negative result does not necessarily rule out the disease.
- Anti-cyclic citrullinated peptide (anti-CCP) test: Anti-CCP is an antibody that is often present in people with RA. A positive anti-CCP test result may indicate the presence of RA, although a negative result does not necessarily rule out the disease.
- Erythrocyte sedimentation rate (ESR) test: The ESR test measures the rate at which red blood cells settle to the bottom of a tube. An elevated ESR may be a sign of inflammation in the body, including RA.
- C-reactive protein (CRP) test: The CRP test measures the level of CRP, a protein produced by the liver that increases in response to inflammation. An elevated CRP level may be a sign of inflammation in the body, including RA.
Imaging Studies
Imaging tests may be used to help diagnose rheumatoid arthritis (RA) and assess the extent of joint damage. These tests may include:
- X-rays: X-rays use radiation to produce images of the bones and joints. X-rays can show changes in the bones and joints that may be caused by RA, such as thinning of the bone, joint space narrowing, and bone erosion.
- Magnetic resonance imaging (MRI): MRI uses a strong magnetic field and radio waves to produce detailed images of the body. MRI can be used to assess the joints, surrounding tissues, and bone for signs of inflammation and damage.
Treatment of Rheumatoid Arthritis
The treatment of rheumatoid arthritis (RA) typically involves a combination of medications, physical therapy, and lifestyle changes. The specific treatment plan will depend on the severity of the disease, the patient’s symptoms, and the patient’s overall health.
Medications
Medications used to treat RA may include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs can help reduce pain and inflammation. Examples include ibuprofen and naproxen.
- Disease-modifying antirheumatic drugs (DMARDs): DMARDs can slow the progression of RA and prevent joint damage by inhibiting certain immune system cells or enzymes that are involved in the inflammation process. Examples include methotrexate, leflunomide, and sulfasalazine.
- Biologics: Biologics are a newer class of medications that target specific proteins involved in the immune response. Examples include tumor necrosis factor (TNF) inhibitors, such as adalimumab and etanercept, and interleukin (IL)-6 inhibitors, such as tocilizumab.
- Corticosteroids: Corticosteroids, such as prednisone, can help reduce inflammation. They may be used as a short-term treatment or in combination with other medications.
Physical Therapy
Physical therapy can help improve joint function, reduce pain, and increase mobility in people with RA. Physical therapy may include exercises to strengthen the muscles around the affected joints, as well as stretching and range of motion exercises.
Lifestyle Changes
Lifestyle changes that may be recommended as part of the treatment of RA include:
- Exercise: Regular physical activity can help reduce pain, improve function, and increase strength.
- Weight management: Maintaining a healthy weight can help reduce the stress on the joints.
- Heat and cold therapy: Applying heat or cold to the affected joints can help reduce pain and stiffness.
- Assistive devices: Using assistive devices, such as canes or splints, can help improve mobility and reduce the strain on the joints.
Prognosis
The prognosis for rheumatoid arthritis (RA) can vary widely and depends on several factors, including the severity of the disease, the patient’s age, and the patient’s overall health.
RA is a chronic autoimmune disease that causes inflammation in the joints and surrounding tissues. Without treatment, RA can cause joint damage and disability. Early diagnosis and treatment can help slow down or stop the progression of the disease and prevent joint damage.
With appropriate treatment, many people with RA are able to manage their symptoms and maintain a good quality of life. However, RA is a chronic condition, and treatment is typically ongoing. It is important for people with RA to work closely with a healthcare provider to develop a treatment plan that is right for them.
Sources
Almutairi, Khalid et al. “The global prevalence of rheumatoid arthritis: a meta-analysis based on a systematic review.” Rheumatology international vol. 41,5 (2021): 863-877. doi:10.1007/s00296-020-04731-0
Bullock, Jacqueline et al. “Rheumatoid Arthritis: A Brief Overview of the Treatment.” Medical principles and practice : international journal of the Kuwait University, Health Science Centre vol. 27,6 (2018): 501-507. doi:10.1159/000493390
Sparks, Jeffrey A. “Rheumatoid Arthritis.” Annals of internal medicine vol. 170,1 (2019): ITC1-ITC16. doi:10.7326/AITC201901010