What are Spinal Fractures?
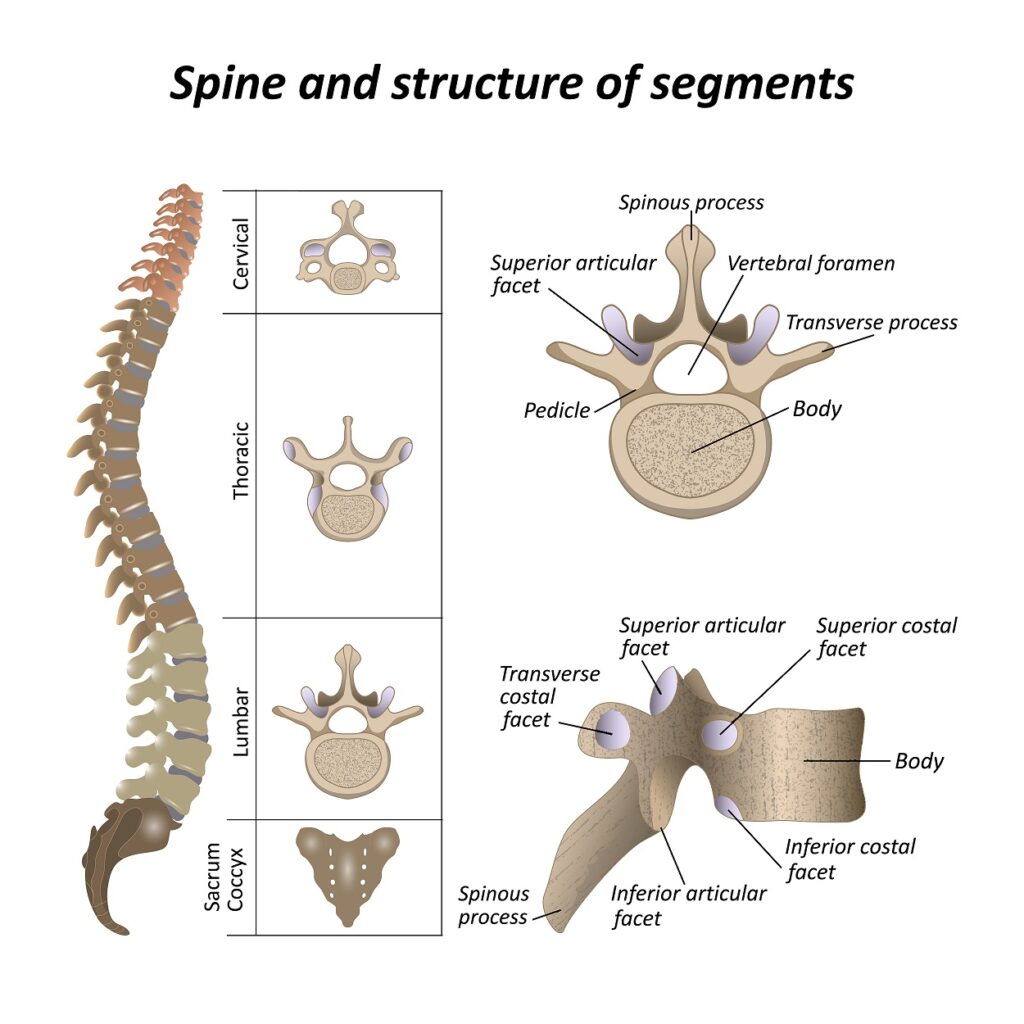
The spine is a column of bones extending from the skull’s base to the pelvis. It is made up of 33 vertebrae, which are separated by intervertebral discs. These bones act as the support structure for the torso and protect the spinal cord as it travels down the body. A spinal fracture occurs when one or more of the vertebrae are broken. This can be the result of trauma, such as a fall or car accident, or due to osteoporosis, which makes the bones weak and brittle. Spinal fractures can be painful and may cause nerve compression or even paralysis. Treatment typically involves rest, bracing, and pain medications. In some cases, surgery may be necessary.
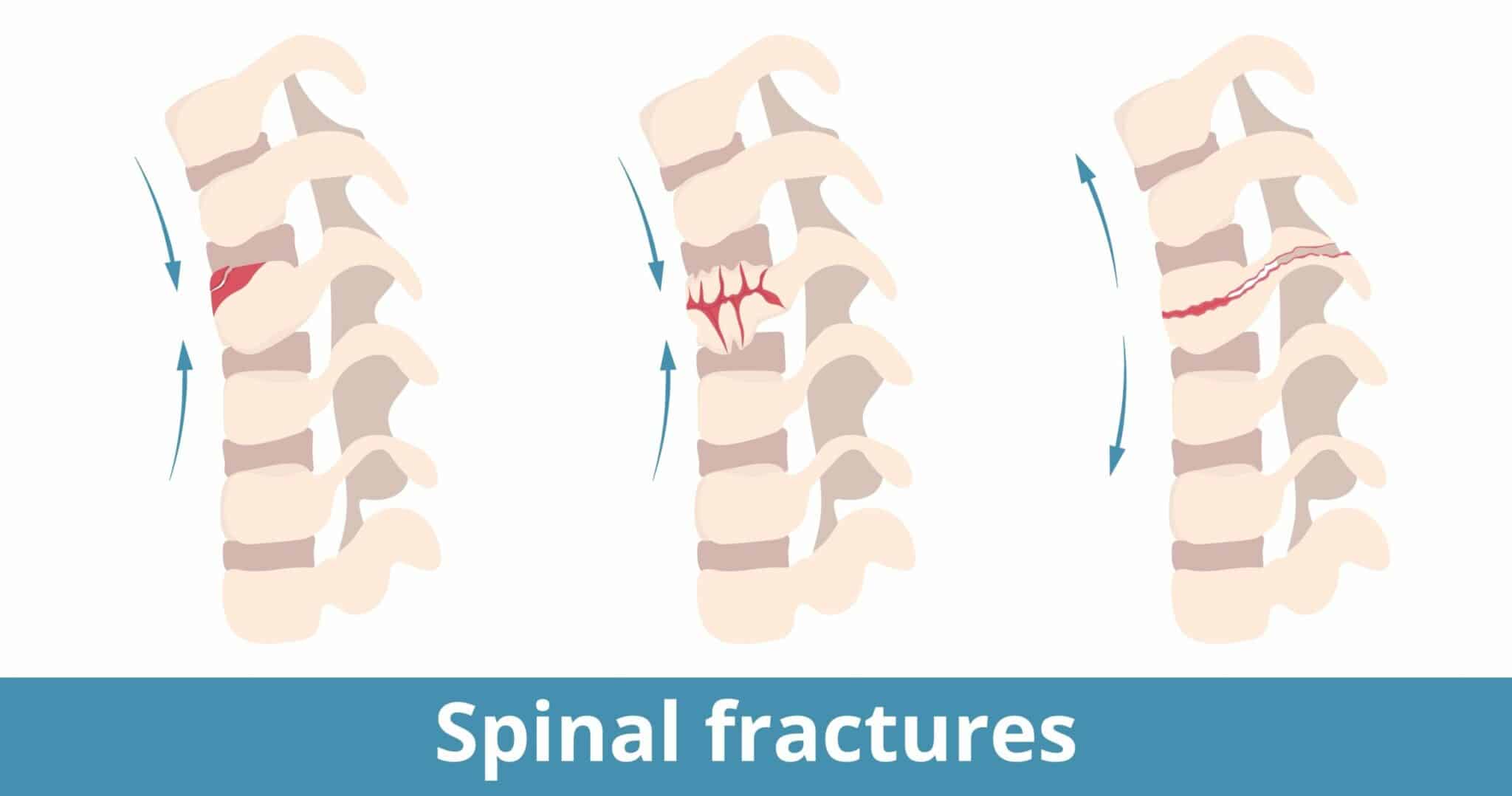
Types of Spinal Fractures
There are several types of spinal fractures that range in severity. Fractures can be thought of as “stable” or “unstable.” Stable fractures have a low risk of bone fragments breaking apart and damaging other structures, such as the spinal cord. Stable fractures are considered less severe. Unstable fractures can result in the spine losing its structural integrity or result in fragments moving around and damaging surrounding structures. There is a risk of spinal cord damage with unstable fractures, so these are considered severe injuries.
Compression and Burst Fractures
A compression fracture occurs when the vertebrae collapses due to fall or impact. This type of fracture is common in people with osteoporosis. Typically, a compression fracture affects the front (anterior) part of the vertebrae and is considered “stable” since the bones usually do not move out of place. On the other hand, a burst fracture occurs when the vertebrae break into multiple pieces. This type of fracture is often more serious, as it can damage the spinal cord and cause severe pain and disability. Spinal fractures can be extremely painful and debilitating, so it is important to get medical help promptly if you think you have fractured your spine. Early diagnosis and treatment can help to minimize the risk of long-term complications.
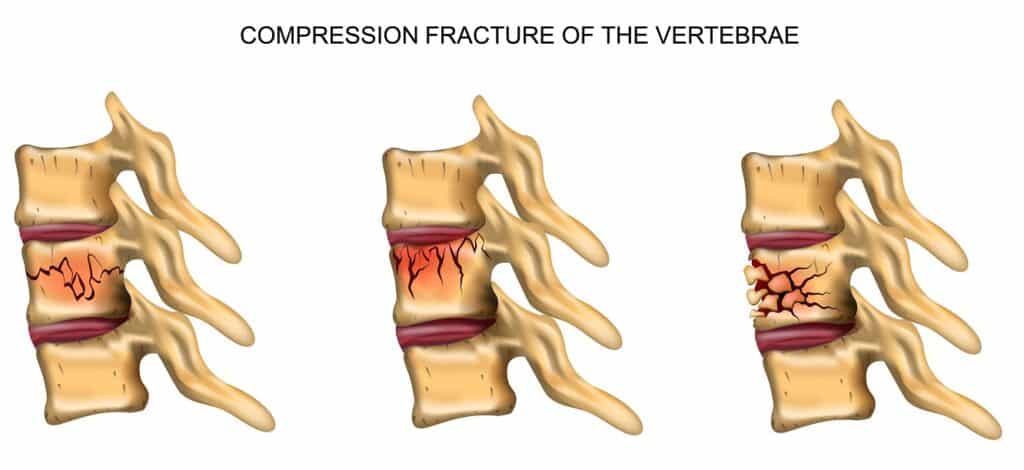
Compression Fracture Grading
Spinal compression fractures are commonly classified based on severity. Each type can be graded semiquantitatively based on the loss of vertebral body height (Genant method).
- Grade 0 (no fracture) describes a typical vertebra.
- Grade 1 (mild fracture) corresponds to a vertebral body height reduced by 20%-25%, with a 10%-20% reduction in surface area compared to the adjacent unaffected vertebra.
- Grade 2 (moderate fracture) corresponds to a vertebral body height reduced by 25%-40%, with a 20%-40% decrease in surface area compared to the adjacent unaffected vertebra.
- Grade 3 (severe fracture) represents a vertebral body height reduced by more than 40%. This system provides a helpful way to compare and contrast different types of fractures.
Flexion/Distraction (Chance) Fractures
Flexion/distraction fractures, also known as “Chance” fractures, occur when there is significant forward force and flexion applied to the spine. This can be seen in a high speed motor vehicle crashes. The force pulls (distracts) the vertebra apart into two pieces. This is typically an unstable fracture.
Transverse Process Fracture
Transverse process fractures occur due to rotational stress on the vertebra. A rapid or extreme twisting motion can cause the tip of this bony prominence to break off where the muscle/ligament attaches. This is considered a stable fracture.
Fracture/Dislocation
If a force is great enough, a vertebral fracture can be accompanied by a dislocation. A dislocation is when the bone slips off the adjacent vertebra and is dislodged from the spinal column. This is an unstable injury.
Causes of Spinal Fractures
Spinal fractures can be caused by a variety of factors, including:
- Trauma or injury: Spinal fractures can result from sudden, traumatic events such as falls, car accidents, sports injuries, or other high-impact accidents.
- Osteoporosis: Osteoporosis is a condition that causes bones to become weak and brittle. In severe cases, it can lead to compression fractures in the spine.
- Cancer: Cancer that has spread to the spine can weaken the bones and make them more prone to fractures.
Incidence of Spinal Fractures
Spinal fractures are relatively common, particularly among older adults. According to the National Osteoporosis Foundation, approximately 700,000 Americans yearly suffer a spinal fracture. Most spinal fractures are caused by osteoporosis, which causes the bones to become porous and brittle. Osteoporosis is most common in postmenopausal women but can also affect men and women of all ages.
Other risk factors for developing osteoporosis include smoking, excessive alcohol consumption, lack of exercise, and certain medications (such as steroids).
Symptoms of Spinal Fractures
The symptoms of a spinal fracture can vary depending on the location and severity of the injury. Some people with spinal fractures may not experience any symptoms at all. However, common symptoms of a spinal fracture may include:
- Back Pain: The most common symptom of a spinal fracture is severe pain in the back that may be worse when standing or walking.
- Numbness or Tingling: A spinal fracture can put pressure on the spinal cord or nerves, causing numbness, tingling, or weakness in the arms or legs.
- Loss of Range of Motion: A spinal fracture can make it difficult to move the back, and may limit the ability to bend or twist.
Diagnosis
A timely diagnosis of a fracture is essential to proper healing. The most common diagnostic method for spinal fractures is an X-ray and CT scan, which can provide detailed information about the location and severity of the fracture. In some instances, an MRI may also be necessary to assess for any spinal cord or ligamentous damage.
Spinal Fracture Treatment Options
The treatment options for spinal fractures depend on the location, grade, and severity of the injury and the patient’s overall health. Generally speaking, treatment may involve a combination of medication, physical therapy, immobilization with a brace, and in severe cases, surgery.
Medication
Non-steroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce inflammation and swelling. Muscle relaxants, such as cyclobenzaprine, may also help reduce pain and improve the range of motion in the affected area.
Bracing
Doctors may recommend wearing a brace to limit movement and protect the spine while it heals. The type of brace or cast used depends on the severity and location of the injury. Still, they are designed to keep the body in an ergonomic position and prevent further damage.
Surgery
The type of surgery used to treat a spinal fracture depends on several factors, including the location and severity of the fracture, the extent of spinal instability, and the patient’s overall health.
Some of the surgical procedures commonly used to treat spinal fractures include:
- Vertebroplasty or Kyphoplasty: A minimally invasive procedure that involves injecting a special cement-like material into the fractured vertebra to stabilize the bone and reduce pain.
- Spinal Fusion: A surgical procedure that joins two or more vertebrae together using bone grafts, rods, screws, or other hardware to stabilize the spine.
- Decompression Surgery: A surgical procedure that relieves pressure on the spinal cord or nerves by removing a portion of the vertebra, herniated disc or other structures that are pressing on them.
The specific type of surgery used to treat a spinal fracture is determined by the patient’s individual needs and the extent of the injury. It’s important to discuss all treatment options with a qualified healthcare provider to determine the best course of action.
Prognosis of Spinal Fractures
The prognosis for a spinal fracture depends on various factors, such as the location and severity of the fracture, the patient’s age and overall health, and the presence of any other injuries or underlying medical conditions.
In general, spinal fractures can range from mild compression fractures that heal on their own with conservative treatment, to more severe fractures that require surgery and can lead to chronic pain or even paralysis.
With prompt and appropriate treatment, many people with spinal fractures can make a good recovery and return to their normal activities. However, some individuals may experience long-term pain or mobility issues.
References
- Kendler, D. L., Bauer, D. C., Davison, K. S., Dian, L., Hanley, D. A., Harris, S. T., McClung, M. R., Miller, P. D., Schousboe, J. T., Yuen, C. K., & Lewiecki, E. M. (2016). Vertebral Fractures: Clinical Importance and Management. The American Journal of Medicine, 129(2), 221.e1–221.e10. https://doi.org/10.1016/j.amjmed.2015.09.020
- Whitney, E., & Alastra, A. J. (2022, May 23). Vertebral Fracture. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK547673/
- Leucht, P., Fischer, K., Muhr, G., & Mueller, E. J. (2009). Epidemiology of traumatic spine fractures. Injury, 40(2), 166–172. https://doi.org/10.1016/j.injury.2008.06.040