Summary
Transverse myelitis is a rare neurological disorder characterized by inflammation of the spinal cord. While its exact cause can vary, autoimmune reactions and infections are common triggers. The symptoms range from motor weakness and sensory changes to pain and loss of bladder control. Accurate diagnosis involves a combination of imaging tests and lumbar puncture. Treatment plans are tailored to each individual’s needs and can include immunotherapy, pain management, and rehabilitation.
Definition of Transverse Myelitis
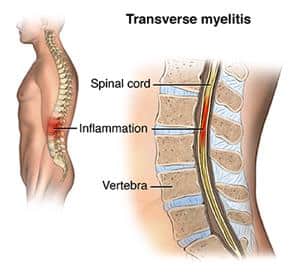
Transverse myelitis is a neurological disorder characterized by inflammation of the spinal cord. The term “transverse” refers to the inflammation extending horizontally across the width of the spinal cord. This inflammation disrupts the normal functioning of nerve fibers, leading to various neurological symptoms. Transverse myelitis is considered a rare condition, but its effects can be significant and life-altering.
Causes of Transverse Myelitis
Transverse myelitis is caused by inflammation of the spinal cord, specifically affecting the cross-sectional (transverse) area of the cord. The exact cause of transverse myelitis can vary from person to person, but there are several factors that have been associated with its development:
- Autoimmune Reactions: In many cases, transverse myelitis is thought to result from an autoimmune reaction, where the body’s immune system mistakenly targets and attacks its own healthy tissues. In this case, the immune response targets the myelin, the protective covering of nerve fibers in the spinal cord. This autoimmune process leads to inflammation and damage, causing the characteristic symptoms of the condition.
- Infections: Infections can trigger an inflammatory response that affects the spinal cord, leading to transverse myelitis. Viral infections are commonly associated with the development of transverse myelitis, including infections caused by herpes viruses, Epstein-Barr virus, enteroviruses, and others. Bacterial infections can also lead to inflammation and subsequent damage to the spinal cord.
- Inflammatory Disorders: Conditions characterized by chronic inflammation, such as multiple sclerosis and neuromyelitis optica, can increase the risk of transverse myelitis. These disorders involve the immune system attacking the central nervous system, including the spinal cord.
- Vaccinations: In rare instances, certain vaccinations have been linked to the development of transverse myelitis. This is thought to occur as an autoimmune reaction triggered by the immune response generated by the vaccine.
Symptoms of Transverse Myelitis
The symptoms of transverse myelitis can vary widely from person to person and depend on the location and extent of the inflammation within the spinal cord. Common symptoms include:
- Motor Weakness: Individuals with transverse myelitis may experience weakness in their arms, legs, or both. This weakness can range from mild to severe and can affect a person’s ability to perform everyday activities.
- Sensory Disturbances: Changes in sensation, such as tingling, numbness, or a “pins and needles” sensation, can occur below the level of the inflammation. These sensations may affect the limbs, trunk, or other areas of the body.
- Pain: Pain is a significant symptom of transverse myelitis. The pain can be sharp, burning, or aching and may occur in the back, neck, or limbs. The pain can be severe and persistent, impacting an individual’s quality of life.
- Loss of Bladder and Bowel Control: Some individuals with transverse myelitis may experience difficulty with bladder and bowel function due to the disruption of nerve signals controlling these processes.
- Spasticity: Muscle stiffness and involuntary muscle contractions, known as spasticity, can occur. This can lead to muscle tightness and difficulty with coordination.
- Difficulty Walking: Due to weakness, sensory changes, and spasticity, walking and maintaining balance can become challenging for those affected by transverse myelitis.
Diagnosis of Transverse Myelitis
Diagnosing transverse myelitis involves a thorough medical evaluation, including medical history assessment, physical examination, and a variety of diagnostic tests. During the physical examination, your healthcare provider will assess your neurological function, motor strength, sensory responses, and reflexes.
Imaging tests such as MRI (Magnetic Resonance Imaging) are crucial for visualizing the spinal cord and identifying inflammation or lesions. These images help rule out other possible causes of symptoms, such as spinal cord compression or tumors. Lumbar puncture (also known as a spinal tap) may be performed to analyze cerebrospinal fluid for signs of inflammation and immune system activity.
Treatment of Transverse Myelitis
The treatment of transverse myelitis aims to reduce inflammation, manage symptoms, and promote rehabilitation. Treatment plans are individualized based on the severity of symptoms and the underlying cause. Some common approaches include:
Immunotherapy
- Corticosteroids: High-dose intravenous corticosteroids, such as methylprednisolone, are often used to suppress inflammation and reduce the immune response. These medications are typically administered early in the course of treatment.
- Intravenous Immunoglobulin (IVIG): IVIG involves infusing immunoglobulin proteins obtained from donated blood. IVIG can help modulate the immune response and may be considered if corticosteroids are not effective or are not well-tolerated.
- Plasmapheresis: Plasmapheresis, also known as plasma exchange, involves removing and filtering a patient’s blood plasma to remove harmful antibodies and immune components. It is sometimes used when other treatments are not providing sufficient relief.
Pain Management
Pain associated with transverse myelitis can be challenging. Various pain management strategies may be employed, including the use of nonsteroidal anti-inflammatory drugs (NSAIDs), anticonvulsants, and certain antidepressants. These medications can help alleviate neuropathic pain and discomfort.
Physical Therapy
Physical therapy plays a vital role in the rehabilitation process for individuals with transverse myelitis. Physical therapists design exercise programs to improve muscle strength, coordination, mobility, and flexibility. Therapy aims to maximize function and independence in daily activities.
Prognosis of Transverse Myelitis
The prognosis of transverse myelitis varies based on factors such as the severity, cause, and promptness of treatment. While some individuals achieve complete recovery with prompt intervention, others experience partial recovery or residual symptoms.
Early diagnosis, appropriate medical care, and ongoing collaboration with healthcare professionals are essential for improving the prognosis and enhancing overall well-being for those affected by transverse myelitis.
The Takeaways
Transverse myelitis is a rare neurological disorder characterized by inflammation of the spinal cord. While its exact cause can vary, autoimmune reactions and infections are common triggers. The symptoms range from motor weakness and sensory changes to pain and loss of bladder control. Accurate diagnosis involves a combination of medical history, physical examination, and imaging tests. Treatment plans are tailored to each individual’s needs and can include immunotherapy, pain management, and rehabilitation. By working closely with healthcare professionals, individuals with transverse myelitis can manage their symptoms and optimize their quality of life. Always seek guidance from a medical expert for personalized diagnosis and treatment recommendations.
Sources
Beh SC, Greenberg BM, Frohman T, Frohman EM. Transverse myelitis. Neurol Clin. 2013;31(1):79-138.
