What is a platelet-rich plasma injection?
Platelet-rich plasma (PRP) injections are a minimally invasive procedure used to treat spine pain caused by damaged intervertebral discs. They are also known as intradiscal platelet-rich plasma injections. This procedure involves injecting concentrated platelets from the patient’s own blood directly into the affected disc under fluoroscopic guidance.
The procedure is typically performed on an outpatient basis and requires only local anesthesia. The effectiveness of intradiscal PRP injections for discogenic back pain is still being studied, and more research is needed to determine its long-term effectiveness.
How do PRP injections work?
Intradiscal platelet-rich plasma (PRP) injections are believed to work by delivering concentrated growth factors directly into the affected disc. The growth factors found in platelets, such as platelet-derived growth factor, transforming growth factor-beta, and insulin-like growth factor, are known to promote tissue repair and regeneration.
When the PRP is injected into the affected disc, it is believed to stimulate the body’s natural healing response, promoting the growth of new cells and tissues. This can lead to reduced inflammation and pain, as well as improved disc function.
Which conditions are treated with PRP?
Intradiscal platelet-rich plasma (PRP) injections are typically used to treat conditions that cause discogenic back pain, which is pain that originates from the spinal discs. Some conditions that may be treated with intradiscal PRP injections include:
- Degenerative Disc Disease: This is a condition in which the spinal discs degenerate over time, leading to pain and decreased mobility.
- Disc Herniation: This occurs when the soft inner material of the disc pushes through a tear in the outer layer, irritating nearby nerves and causing pain.
What to expect during the procedure
The procedure for intradiscal platelet-rich plasma (PRP) injections typically involves the following steps:
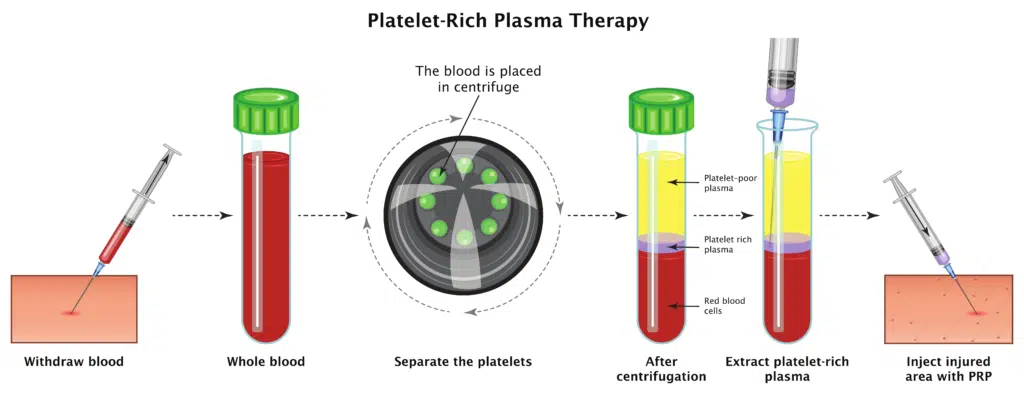
- Blood Draw: A small amount of the patient’s own blood is drawn and placed into a special tube designed to separate the platelets from the other components of the blood.
- Platelet Separation: The tube of blood is placed in a centrifuge, which spins the blood at a high speed to separate the platelets from the other blood components.
- Preparation: The patient is positioned on the exam table, and the area around the injection site is cleaned and sterilized.
- Local Anesthesia: The skin and deeper tissues surrounding the injection site are numbed with a local anesthetic to minimize pain and discomfort during the procedure.
- PRP Injection: The concentrated PRP is drawn up into a syringe and injected directly into the affected spinal disc under fluoroscopic guidance. The injection is typically performed using a thin needle.
- Post-Injection Monitoring: After the injection, the patient is monitored for a short period to ensure that there are no immediate complications or adverse reactions to the procedure.
The entire procedure typically takes less than an hour to complete and can be performed on an outpatient basis.
What is the recovery time?
Most patients are able to resume their normal activities within a few days following the procedure.
However, Patients may experience some soreness or stiffness at the injection site for a few days following the procedure. To help manage these symptoms, patients may be advised to apply ice to the injection site for short periods of time or take over-the-counter pain medications as directed by their healthcare provider.
How long do PRP injections take to work?
The timeline for when patients may experience relief from their symptoms following intradiscal platelet-rich plasma (PRP) injections can vary. Some patients may experience an improvement in their symptoms within a few days or weeks of the procedure, while others may take several weeks or months to see an improvement.
What are the risks of PRP injections?
As with any medical procedure, intradiscal platelet-rich plasma (PRP) injections do carry some risks and potential complications. Some of the risks associated with this procedure may include:
- Infection: As with any invasive procedure, there is a risk of infection at the injection site. Patients may be prescribed antibiotics before and after the procedure to help prevent infection.
- Bleeding: The injection may cause some bleeding in the disc or surrounding tissues. Patients taking blood-thinning medications may be at a higher risk for bleeding complications.
- Nerve Injury: There is a small risk of nerve injury or damage to the spinal cord or surrounding nerves. Patients may experience numbness, weakness, or tingling in the legs or arms if this occurs.
Do PRP injections work?
Intradiscal platelet-rich plasma (PRP) injections have shown promising results in some studies for the treatment of discogenic back pain (Levi 2016). However, there is limited research on this treatment and more studies are needed.
According the the North American Spine Society (NASS), there is insufficient evidence to make a recommendation for or against the use of intradiscal platelet rich plasma in patients with discogenic low back pain.
Are intradiscal PRP injections right for me?
Intradiscal PRP injections are typically recommended for patients with chronic discogenic back pain who have not responded to other treatments, such as physical therapy, medications, or spinal injections.
Patients considering this procedure should discuss the potential risks and benefits with their healthcare provider. It is important to note that intradiscal PRP injections are not currently considered a standard treatment option and may not be covered by insurance.
Citations
Levi, David et al. “Intradiscal Platelet-Rich Plasma Injection for Chronic Discogenic Low Back Pain: Preliminary Results from a Prospective Trial.” Pain medicine (Malden, Mass.) vol. 17,6 (2016): 1010-22. doi:10.1093/pm/pnv053
