A herniated disc is when the intervertebral disc ruptures, spilling its jelly like center into the spinal canal. It often occurs due to age-related degeneration but can also be caused by traumatic injury. The symptoms of a herniated disc include pain, numbness, and weakness, depending on the location of the herniation and which nerves are affected. Treatments vary based on the severity of the herniation, and can range from pain control and physical therapy to surgery.
Anatomical Structure of Intervertebral Discs
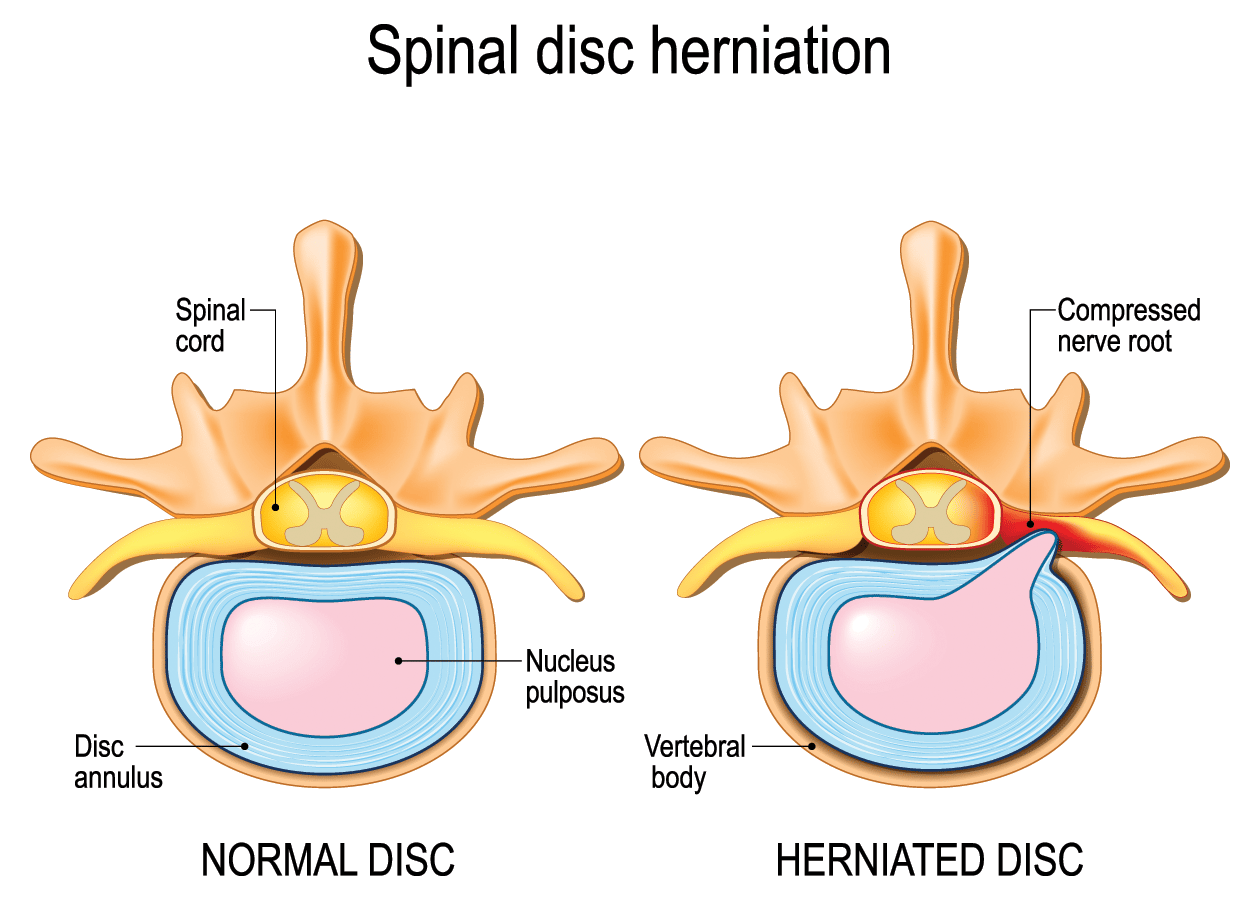
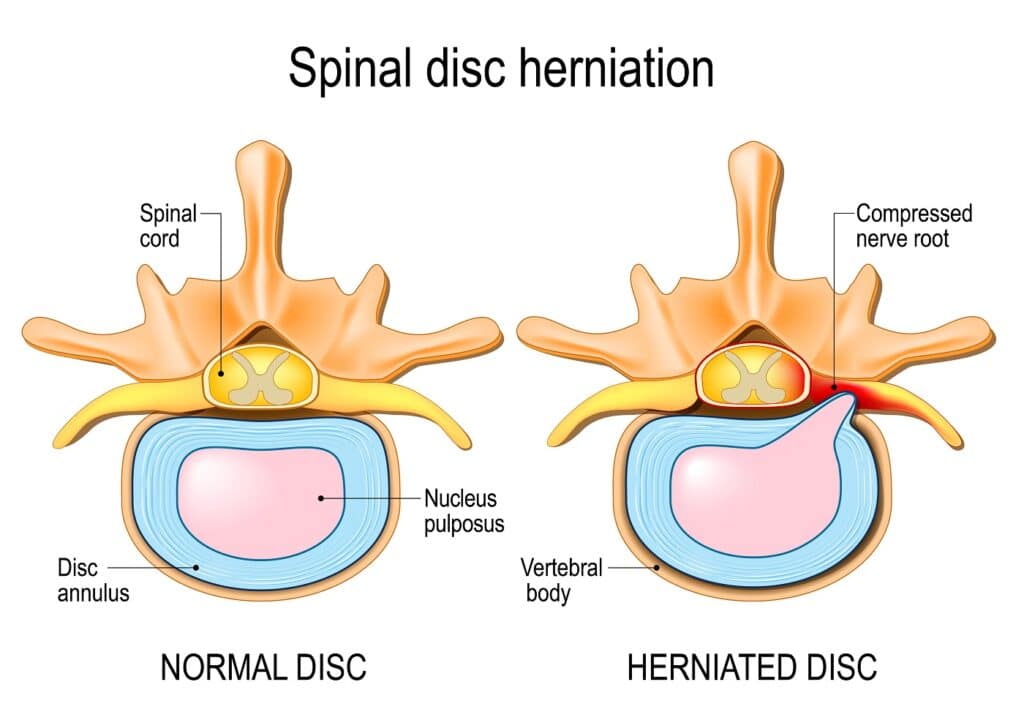
The spine is made up of 33 vertebral bones separated by intervertebral discs. Discs are made of strong fibrous tissue on the outside (annulus fibrosis, or AF) and a soft jelly-like center (nucleus pulposus, or NP). The annulus is thickest at its lateral margins (outer edges) but thins out toward its center. This allows flexibility in bending while maintaining stability against compressive forces acting on the vertebral bodies. The annulus encases the nucleus pulposus, which is a jelly like substance that contains 80% water by weight.
The discs primarily function as shock absorbers for the spine distributing compressive forces. They also allow the spine to be supportive yet flexible, and provide space between each vertebra for spinal nerves to exit.
What is a Herniated Disc?
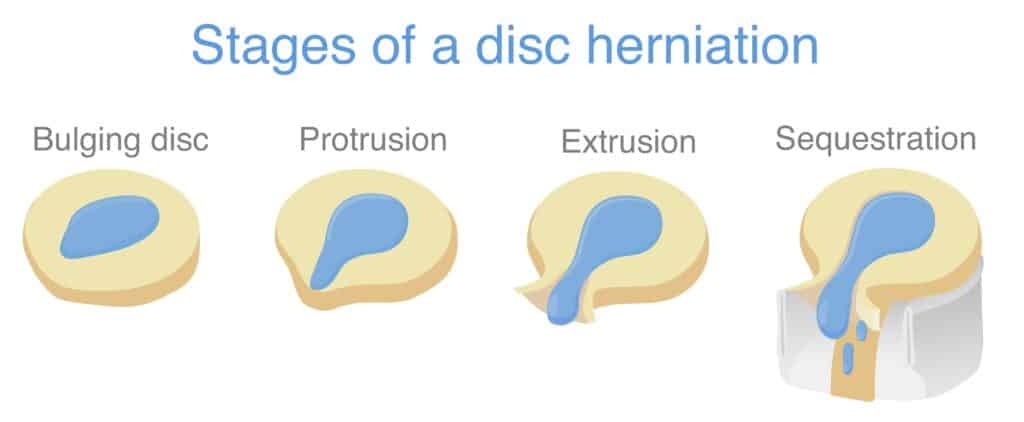
A herniated disc is when the intervertebral disc ruptures, spilling its jelly-like center into the spinal canal. Different terms are used to express the variances in appearance and the severity of different types of herniations.
Disc bulge: A disc bulge is not a true herniation, but instead a broad based ballooning of the disc into the spinal canal. It is caused by weakening of the outside layer of the spinal disc (called the annulus), causing the disc to flatten and balloon out. A disc bulge is less severe than a disc herniation, where the annulus breaks and the nucleus spills out.
Disc protrusion: A disc protrusion describes the appearance of a herniation in which the disc material prolapses out. Specifically, it is when the base of the herniation is wider than tip of the herniation.
Disc extrusion: A disc extrusion is when the disc material of the herniation is wider at the tip than at the base.
Disc sequestration: A disc sequestration is when the herniated disc material loses continuity with the disc and is completely separated.
What Are The Possible Causes of a Herniated Disc?
There are several potential causes of a disc herniation in the spine. Some of the most common causes include:
- Age-related degeneration: As we age, the intervertebral discs in our spine can begin to break down and lose their elasticity. This can lead to a disc herniation.
- Trauma: A sudden injury or impact to the spine, such as from a car accident or a fall, can cause a disc herniation.
- Overuse injuries: Repeated strain on the spine, such as from heavy lifting or repetitive motions, can cause a disc herniation over time.
- Poor posture: Poor posture, such as slouching or hunching over a desk or computer, can put excess strain on the spine and lead to a disc herniation.
- Obesity: Carrying excess weight can put additional pressure on the spine and increase the risk of a disc herniation.
It’s worth noting that not all disc herniations are caused by one specific factor. In many cases, a combination of factors may contribute to the development of a disc herniation.
Herniated Disc Symptoms
Symptoms of a herniated disc depend on the location and severity of the herniation.
If the herniated disc is in the neck (cervical spine), you may experience:
- Neck pain
- Arm pain
- Arm numbness/ tingling
- Arm weakness
If the herniated disc is in the low back (lumbar spine), you may experience:
- Back pain
- Buttock pain
- Leg pain
- Leg numbness/tingling
- Leg weakness
Rarely, a severe herniation may cause a condition called cauda equina syndrome (CES), nerve compression that can result in permanent neurological damage including paralysis.
The following symptoms are suggesting of CES and require immediate medical attention:
- Numbness in your private area (saddle anesthesia)
- Bowel or bladder incontinence
- Weakness or numbness affecting both of your legs
Incidence
The incidence of a herniated disc is about 5 to 20 cases per 1000 adults annually and is most common in people in their 30s to 50s. Men are twice as likely to suffer from a herniated disc than women.
Diagnosis
A herniated disc is typically diagnosed through a combination of medical history, physical examination, and imaging tests.
History and Physical Examination
During the medical history, your doctor will ask about your symptoms, including the location and type of pain you’re experiencing, as well as any other relevant medical conditions. Your doctor will also perform a physical examination to assess your range of motion, muscle strength, and reflexes.
Imaging Studies
Imaging tests are typically used to confirm the diagnosis of a herniated disc and to determine the location and extent of the injury. The most common imaging tests used to diagnose a herniated disc are:
- X-ray: This test uses radiation to produce images of the spine. While x-rays can show the bones of the spine, they cannot show the intervertebral discs.
- Magnetic resonance imaging (MRI): This test uses a strong magnetic field and radio waves to produce detailed images of the spine. MRI is often the preferred imaging test for diagnosing a herniated disc because it can show the soft tissues, including the intervertebral discs, in great detail.
- Computed tomography (CT) scan: This test uses X-rays and a computer to produce detailed cross-sectional images of the spine. Like MRI, CT scans can show the bones and soft tissues of the spine.
It’s important to note that a herniated disc can sometimes be present without causing any symptoms. In these cases, the condition may be discovered during imaging tests done for other reasons.
Treatments
Often, symptoms from a herniated disc improved with conservative measures such as pain control and physical therapy. In severe cases, a surgery may be indicated.
Non-surgical Treatment Options
Non surgical treatment options for a herniated disc include:
- Pain control with medications such as non-steroidal anti-inflammatories (NSAIDs) like ibuprofen
- Physical therapy
- Epidural steroid injections
These are usually reserved for treating mild to moderate herniated disc cases.
Surgical Treatment Options
Surgical treatment is typically reserved for severe cases and those that do not improve with conservative management. Surgery is performed to decompress the nerve and remove damaged disc.
A laminectomy removes part of the vertebra, known as the lamina, which acts as the roof of the spinal cord. This helps decompress the nerves.
A discectomy removes abnormal disc material that may be pressing on the spinal cord or nerve roots.
Summary
A herniated disc is when the intervertebral disc ruptures, spilling its jelly like center into the spinal canal. It often occurs due to age-related degeneration but can also be caused by traumatic injury. The symptoms of a herniated disc include pain, numbness, and weakness, depending on the location of the herniation and which nerves are affected. Treatments vary based on the severity of the herniation, and can range from pain control and physical therapy to surgery.
References
Fardon, David F et al. “Lumbar disc nomenclature: version 2.0: Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology.” The spine journal : official journal of the North American Spine Societyvol. 14,11 (2014): 2525-45. doi:10.1016/j.spinee.2014.04.022
Kreiner, D Scott et al. “An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy.” The spine journal : official journal of the North American Spine Societyvol. 14,1 (2014): 180-91. doi:10.1016/j.spinee.2013.08.003
Waxenbaum JA, Reddy V, Futterman B. Anatomy, Back, Intervertebral Discs. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470583/
Dydyk AM, Ngnitewe Massa R, Mesfin FB. Disc Herniation. [Updated 2022 Jan 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/