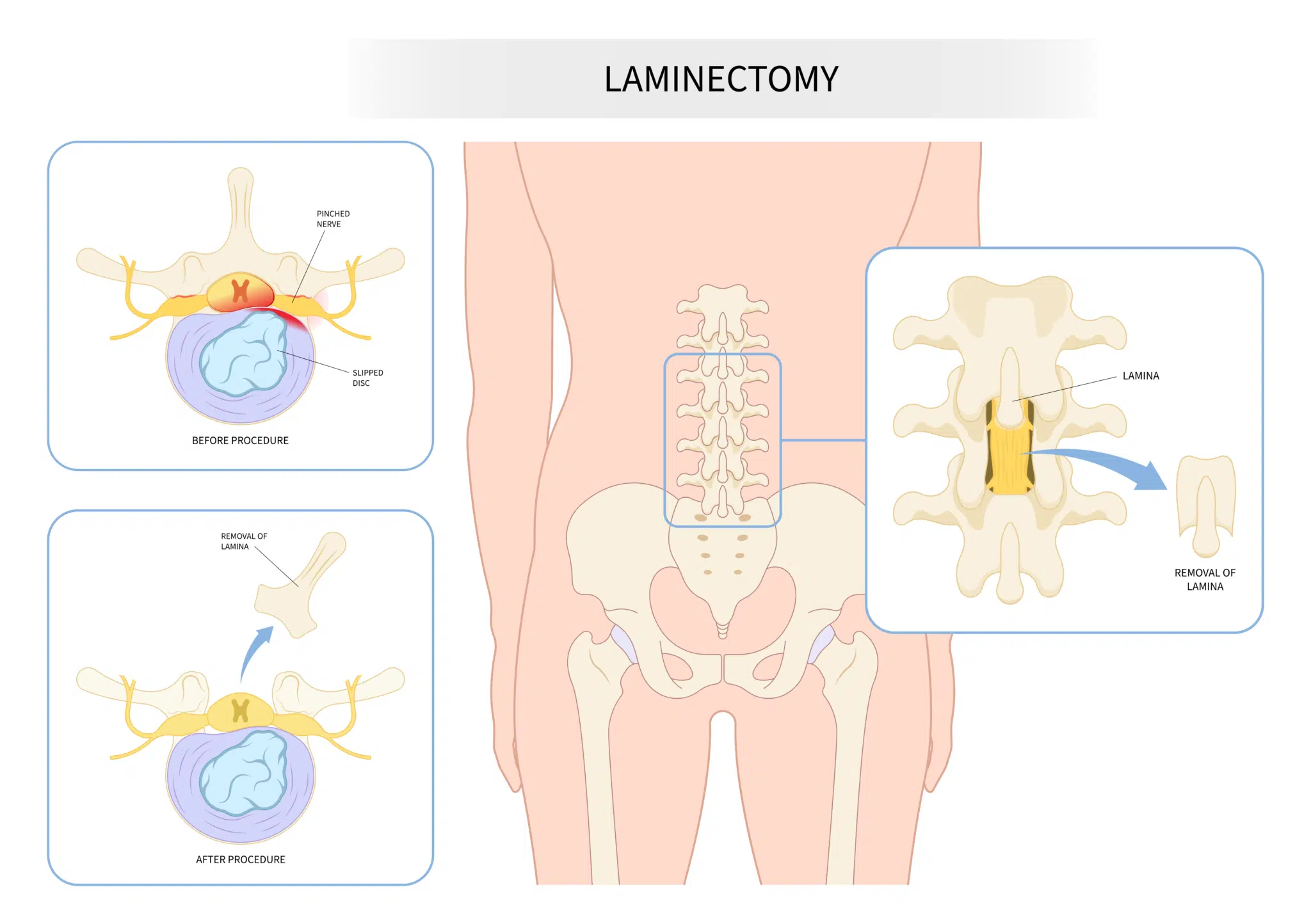
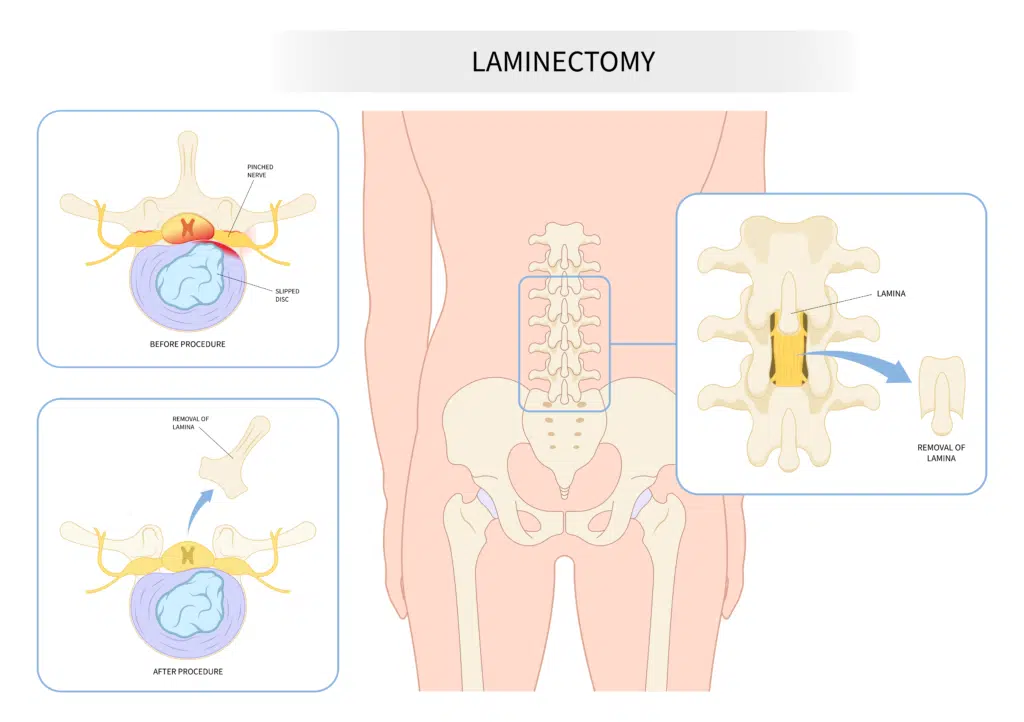
A laminectomy is a type of spine surgery that involves surgical removal of a segment of bone called the lamina. The lamina is the arch that forms the roof of the spinal canal. Removing this roof creates space and can relieve pressure on the spinal cord or nerve roots. This procedure is often done to treat conditions such as spinal stenosis, or provide access to herniated discs and tumors of the spinal cord.
What is a laminectomy?
The spine is made up of a series of stacked bones linked in a chain. Each segment is called a vertebrae. A major function of these bones is to convey the spinal cord through a protective tunnel called the spinal canal. The lamina forms the roof of this tunnel. Shaped a bit like a large wishbone, it is the part of the vertebra that sits above the spinal cord and nerve roots. Lamina stack together in a similar manner to a row of roof tiles. It is sometimes necessary to remove the lamina to decompress the spinal cord and nerve roots, or to create a corridor to access deeper structures. This procedure is called a laminectomy.
When is a laminectomy considered?
A laminectomy directly treats narrowing of the spinal canal (also known as spinal stenosis), or may be an initial step of a multi-step procedure. Surgery is typically a treatment of last resort in patients whose symptoms were not adequately controlled with measures such as physical therapy, medications, or epidural injections.
Some conditions in which laminectomy may be amenable include:
- Herniated discs: A herniated, or ruptured, disc is a condition in which the outer layer of a disc (annulus) breaks and the gel-like contents (nucleus pulposus) push into the canal.
- Degenerative changes: Wear and tear can cause degenerative changes in the spine, just as elsewhere in the body. This can lead to bony growths (called “osteophytes”), or thickened ligaments, which can contribute to canal narrowing.
- Tumors: Tumors or other abnormal growths can grow to cause crowding of the spinal canal and compression of nervous tissue .
How is a laminectomy performed?
A laminectomy is typically done under general anesthesia and can be performed as an open surgery or minimally invasive surgery.
Open laminectomy
During an open laminectomy, the surgeon will make an incision in the back, and then use specialized instruments to remove the portion of the lamina that is pressing on the spinal cord or nerve roots. In some cases, the surgeon may also remove any surrounding tissue, such as a herniated disc, that is putting pressure on the spinal cord or nerve roots. The incision is then closed with sutures or staples.
Minimally invasive laminectomy
Minimally invasive (abbreviated MIS) laminectomy describes a collection of techniques which seek to minimize tissue damage above the site of the laminectomy. The term is not well-defined, and may refer to using smaller-than-normal retractors (“mini-open”), tubular muscle dilators together with microscope (“tubular MIS”), or endoscopic approaches which use a small camera on the end of a long tube. Each technique has unique advantages and disadvantages that should be discussed with your surgeon.
What is the recovery time?
Recovery time after a laminectomy can vary depending on the extent of the surgery and the patient’s overall health.
In many cases, patients can be discharged home the day of surgery. Other patients may expect to spend several days in the hospital after the surgery. Physical therapy is often recommended to help the patient regain strength and mobility, and the patient will be encouraged to get up and move around as soon as possible to prevent blood clots and improve circulation.
After being discharged from the hospital, patients can expect to take several weeks to several months to fully recover. Most patients are able to return to their normal activities within a few weeks after surgery.
What are the risks of a laminectomy?
As with any surgical procedure, a laminectomy carries certain risks that should be considered. Some of these include:
- Bleeding: There is a risk of bleeding during or after the surgery.
- Infection: As with any surgical procedure, there is a risk of infection at the surgical site.
- CSF leak: Clear fluid bathes the spinal cord and nerve roots. This fluid is called cerebrospinal fluid (or “CSF”) and is contained in a covering called the dura. Sometimes, laminectomy can lead to a hole in the dura through which CSF can leak out. Durotomy are frequently able to be repaired at the time of surgery; however, they can lead to headaches, issues with wound healing, or nerve root inflammation.
- Adjacent segment disease: removing the lamina can cause instability in the spine, leading to the degeneration of the adjacent segment which can lead to further pain, spinal cord compression and other symptoms. This may require additional surgery.
- Persistent or new pain: Some patients may experience persistent or new pain after the surgery.
- Spinal cord or nerve root injury: there is a risk of injury to the spinal cord or nerve roots during the surgery, which can lead to new or worsening symptoms.
How effective is a laminectomy?
The effectiveness of a laminectomy can vary depending on the underlying condition and the extent of the compression, however studies have shown patient satisfaction greater than 70% of the time (Phan 2016).
Is a laminectomy right for me?
The decision to undergo a laminectomy is typically made on a case-by-case basis after a thorough evaluation of the patient’s symptoms, diagnostic test results, and overall health.
Here are some factors that may be taken into consideration when determining if a laminectomy is the right treatment option for you:
- Symptoms: If you are experiencing pain, numbness, tingling, or weakness in your legs or arms caused by compression of the spinal cord or nerve roots, a laminectomy may be considered.
- Previous treatment: If more conservative treatments such as physical therapy, medications, or epidural injections have failed to provide relief, a laminectomy may be considered.
- Overall health: Your surgeon will consider your overall health and any other medical conditions you may have to determine if you are a good candidate for surgery.
- Capacity for postoperative rehabilitation: Laminectomy usually works best when paired with the right physical therapy. If you can’t stick with the prescribed therapy plan, it might not be as effective.
It’s important to have a thorough discussion with your surgeon about all the potential options, their risks and benefits, as well as the recovery time and outcomes. This will help you make an informed decision about the best course of treatment for you.