Spinal arachnoiditis is a rare but debilitating condition that affects the delicate membranes surrounding the spinal cord. It involves inflammation of the arachnoid, one of the layers of tissue that protect the spinal cord and nerve roots. This article aims to provide a comprehensive overview of spinal arachnoiditis, including its causes, symptoms, and available treatment options.
What is arachnoiditis?
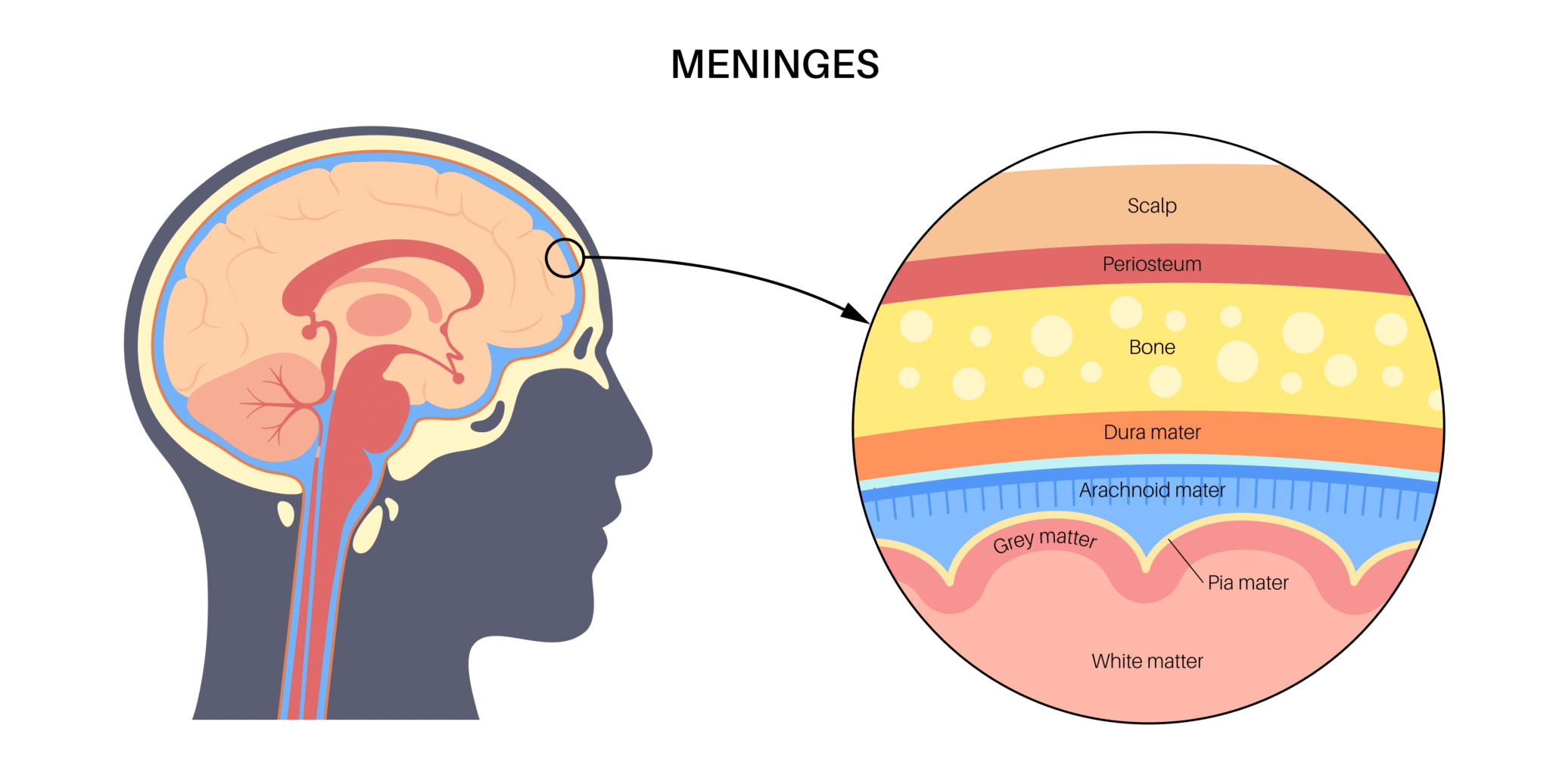
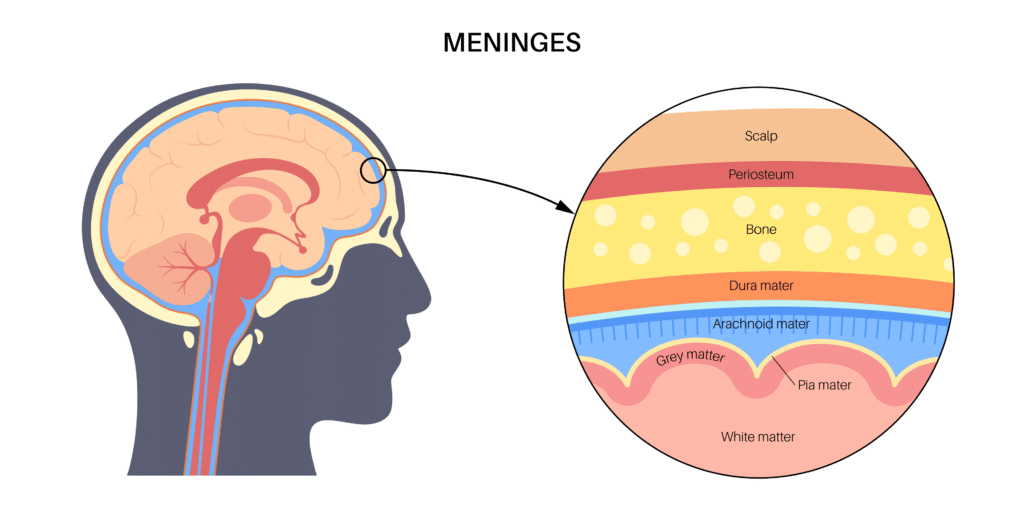
Arachnoiditis is a condition characterized by inflammation of the arachnoid membrane, which is one of the three protective layers (meninges) that surround and encase the brain and spinal cord. The arachnoid membrane lies between the outermost dura mater and the innermost pia mater.
What causes arachnoiditis?
Arachnoiditis can be caused by various factors that lead to inflammation and damage to the arachnoid membrane. These causes include:
- Infections: Bacterial, viral, or fungal infections can trigger arachnoiditis. Examples include meningitis (inflammation of the meninges), tuberculosis, or infections related to spinal surgery.
- Chemical irritation: Certain substances or chemicals can cause inflammation and damage to the arachnoid membrane. These may include myelography dyes (used in diagnostic imaging procedures), epidural steroid injections, or contrast agents used in imaging tests.
- Trauma: Physical injury to the spine or spinal surgeries can result in arachnoiditis. The trauma can cause scarring, adhesions, or direct damage to the arachnoid membrane.
- Chronic compression: Conditions that lead to prolonged compression or irritation of the spinal cord and nerve roots can contribute to the development of arachnoiditis. These may include spinal stenosis (narrowing of the spinal canal), herniated discs, or spinal tumors.
- Spinal interventions: Repeated spinal procedures, such as multiple spinal surgeries or multiple lumbar punctures (spinal taps), can increase the risk of developing arachnoiditis.
It’s important to note that while these factors are known to be associated with arachnoiditis, the condition can sometimes occur spontaneously without a clearly identifiable cause.
What are the symptoms of arachnoiditis?
Arachnoiditis can present with a variety of symptoms that can vary in severity and progression. The symptoms of arachnoiditis may include:
- Chronic pain: Persistent and often severe pain is a hallmark symptom of arachnoiditis. The pain may be localized to the lower back, legs, or buttocks. It can be described as sharp, burning, or shooting in nature. The pain may worsen with movement, prolonged sitting or standing, or certain activities.
- Numbness and tingling: Individuals with arachnoiditis may experience sensations of numbness, tingling, or “pins and needles” in the affected areas. These sensations typically occur in the lower extremities but can also affect other parts of the body.
- Muscle weakness: Weakness in the legs or difficulty in walking can develop as arachnoiditis progresses. The affected muscles may feel weak or fatigued, leading to problems with coordination and mobility.
- Sensory disturbances: Arachnoiditis can cause alterations in sensory perception. This can manifest as increased sensitivity to touch (hyperesthesia) or decreased sensation in the affected areas.
- Bladder and bowel dysfunction: Arachnoiditis can disrupt the normal functioning of the nerves that control bladder and bowel function. This can lead to urinary incontinence (inability to control urine flow), difficulty emptying the bladder completely, or bowel disturbances such as constipation.
- Sexual dysfunction: Some individuals with arachnoiditis may experience sexual dysfunction, including decreased libido, erectile dysfunction, or difficulties with sexual arousal or orgasm.
How is arachnoiditis diagnosed?
Diagnosing arachnoiditis can be challenging as there is no single definitive test for its diagnosis. Instead, healthcare professionals rely on a combination of clinical presentation, symptoms, and imaging studies to reach a diagnosis.
- Clinical Presentation: The diagnosis of arachnoiditis is often based on your symptoms, physical examination findings, and your clinical history of potential triggering events.
- Imaging Studies: The primary imaging modality used for diagnosing arachnoiditis is magnetic resonance imaging (MRI). MRI scans can provide detailed images of the spinal cord and surrounding structures. Typical findings may include loculated arachnoid cysts, spinal cord swelling, cord displacement, nerve root clumping, syrinx formation, and arachnoid septations. Computed tomography (CT) myelography can also be used to visualize the spinal cord and nerve roots. It may reveal blockage of contrast spread, thickened or tethered nerve roots, soft tissue masses, or intrathecal calcification.
It is important to note that a diagnosis of arachnoiditis is made based on a combination of your symptoms, clinical history, physical examination, and imaging findings consistent with arachnoiditis. MRI has high sensitivity, specificity, and accuracy for diagnosing chronic adhesive arachnoiditis. However, there may be cases where MRI is inconclusive, and additional procedures such as thecaloscopy or spinal cord biopsy may be considered to aid in the diagnosis.
What is the treatment for arachnoiditis?
Arachnoiditis is a challenging and incurable condition that requires a comprehensive treatment approach. The primary goal of treatment is to alleviate pain, improve quality of life, and manage symptoms. Let’s explore the various treatment options available to help patients cope with their condition.
- Medication Management: To manage pain and related symptoms, different medications may be prescribed. These can include nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation, opioids for severe pain, and adjunct medications such as duloxetine, gabapentin, pregabalin, and muscle relaxants like baclofen. The selection of medications is personalized based on individual needs and response.
- Physical Therapy: Physical therapy plays a crucial role in managing arachnoiditis. A physical therapist can design a customized exercise program to improve strength, flexibility, and overall physical function. Physical therapy techniques may include exercises, stretches, and techniques to improve posture and body mechanics.
- Psychological Support: Managing the emotional impact of arachnoiditis is essential. Cognitive behavioral therapy, biofeedback, imagery, and other forms of psychotherapy can help patients cope with pain, reduce stress, and improve overall well-being. Seeking support from therapists or joining support groups may also provide valuable emotional support.
- Surgical Interventions: Surgical treatment options for arachnoiditis are limited and usually reserved for specific situations. Surgical interventions may involve releasing a tethered cord, restoring cerebrospinal fluid (CSF) flow, or addressing complications like epidural infection. However, surgical outcomes for arachnoiditis are generally poor, and the benefits may be temporary.
- Assistive Devices: Motorized assistant devices, such as standing wheelchairs, may benefit patients who have difficulty sitting due to pain. These devices can improve mobility and overall quality of life. However, it’s important to evaluate the patient’s tolerance and endurance for standing before considering such devices.
It’s worth noting that epidural steroid injections are generally not recommended for arachnoiditis due to concerns about potential exacerbation of symptoms. Oral corticosteroids have also not shown therapeutic benefit for arachnoiditis.
What is the prognosis for arachnoiditis?
Arachnoiditis is generally considered a chronic and incurable disease, which means that complete resolution of symptoms is unlikely. The severity of symptoms can vary, ranging from mild to severe, and this can influence an individual’s ability to perform daily activities and participate in certain aspects of life. Managing pain and functional limitations is a key focus of treatment to improve overall well-being.
Conclusion
Spinal arachnoiditis is a complex and debilitating condition that affects the arachnoid membrane surrounding the spinal cord. While there is no cure, various treatment options exist to manage symptoms and improve the overall well-being of those affected. Early diagnosis,proper medical management, and a multidisciplinary approach involving healthcare professionals specializing in pain management, neurology, and rehabilitation can significantly help individuals with spinal arachnoiditis in managing their condition and improving their quality of life.