Summary
Lateral recess stenosis refers to the narrowing of the lateral recess in the spinal canal, often caused by factors like degeneration, herniated discs, arthritis, or congenital factors. Common symptoms include back pain, leg pain, numbness, and weakness. Diagnosis involves a thorough evaluation, including medical history, physical examination, and imaging studies like MRI. Treatment options vary based on severity, ranging from conservative approaches like physical therapy and medication to more invasive procedures. In severe cases or when conservative methods fail, surgery, such as laminectomy or discectomy, may be considered to relieve nerve compression and alleviate symptoms.
What is Lateral Recess Stenosis?
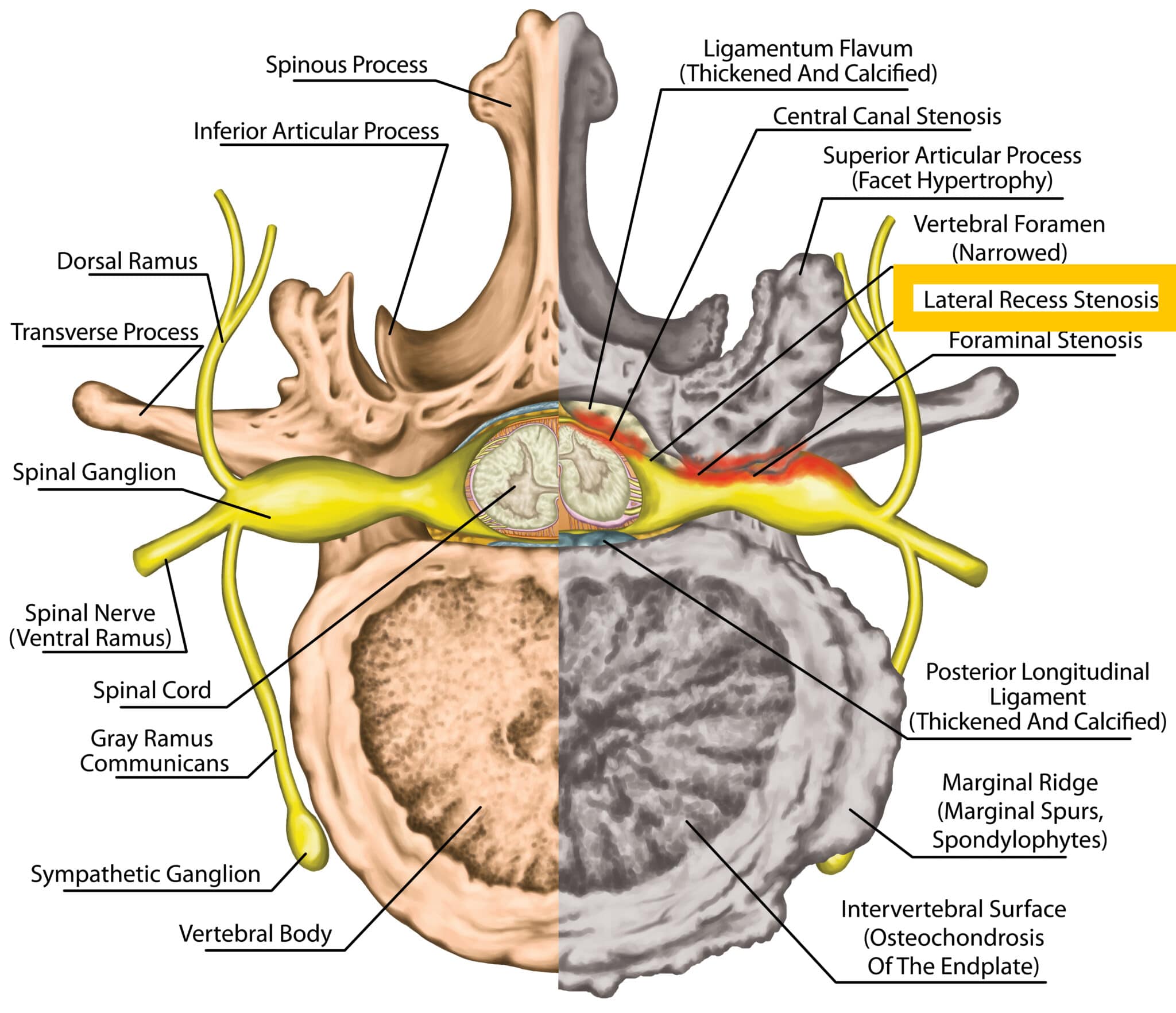
To better understand this term, it’s important to understand some spinal anatomy.
The spinal canal, also known as the vertebral or spinal foramen, is a hollow, bony channel that runs through the vertebral column, providing protection for the spinal cord. The spinal canal has various structural components, including the central canal, lateral recesses, and neural foramina.
The central canal contains the spinal cord itself, while the neural foramina are openings on both sides of the spinal canal through which spinal nerve roots exit. The lateral recess is the area of the canal closest to the sides, just before the neural foramina.
Lateral recess stenosis is the narrowing of the lateral recess.
Causes of Lateral Recess Stenosis
Several factors contribute to the development of lateral recess stenosis:
- Degenerative Changes: The most common cause is age-related degeneration of the spine, which can lead to the thickening of ligaments, the formation of bone spurs, and the collapse of intervertebral discs, all of which can narrow the lateral recesses.
- Herniated Discs: When the gel-like material within the intervertebral discs bulges or ruptures, it can push against the lateral recesses and compress nerve roots.
- Arthritis: Conditions like osteoarthritis and rheumatoid arthritis can lead to inflammation and the growth of bone spurs that impinge on the lateral recesses.
- Congenital Factors: In some cases, individuals may have a narrower spinal canal due to genetics, making them more susceptible to developing lateral recess stenosis.
Symptoms of Lateral Recess Stenosis
The symptoms of lateral recess stenosis can vary depending on the severity and location of the compression. Common symptoms include:
- Back Pain: Dull or aching pain in the lower back is often the initial symptom.
- Leg Pain: Sharp, shooting pain radiating down one or both legs, known as sciatica, is a hallmark symptom.
- Numbness and Tingling: You may experience sensations of numbness or tingling in the legs or feet.
- Weakness: Muscle weakness, particularly in the legs, can occur as nerve compression progresses.
Diagnosing Lateral Recess Stenosis
To diagnose lateral recess stenosis, your healthcare provider will perform a thorough evaluation, which may include:
- Medical History: Discussing your symptoms and medical history to identify potential risk factors.
- Physical Examination: Assessing your range of motion, reflexes, and muscle strength.
- Imaging Studies: X-rays, MRI (Magnetic Resonance Imaging), or CT (Computed Tomography) scans may be ordered to visualize the spine and confirm the diagnosis. MRI is considered the gold standard test. MRI is a highly effective tool for visualizing soft tissues, including the spinal cord, nerve roots, and any structural abnormalities. It can provide detailed images of the spinal canal and neural foramina, allowing healthcare providers to assess the extent of nerve compression.
Treatment of Lateral Recess Stenosis
The treatment of lateral recess stenosis depends on the severity of the condition, the specific symptoms, and the underlying cause. Treatment options can range from conservative approaches to more invasive interventions.
Conservative Treatments
Physical Therapy: Physical therapy can help improve your strength, flexibility, and posture. A physical therapist can design a tailored exercise program to alleviate pain, improve mobility, and provide education on proper body mechanics.
Medications: Over-the-counter or prescription medications may be recommended to manage pain, inflammation, and muscle spasms. Common medications include nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and other pain medications.
Epidural Steroid Injections
In some cases, corticosteroid injections into the epidural space around the affected nerve roots can provide temporary relief by reducing inflammation and pain.
Surgical Treatments
In situations marked by severe symptoms and substantial nerve compression, or in instances where conservative treatments have proven ineffective, surgical intervention may be considered.
Such surgeries include:
Laminectomy: This surgical procedure involves removing a portion of the vertebral bone to create more space within the spinal canal and relieve pressure on the nerve roots.
Discectomy: If the stenosis is caused by a herniated disc, a discectomy may be performed to remove part or all of a damaged intervertebral disc in the spine.
Conclusion
Lateral recess stenosis is a condition characterized by the narrowing of the lateral recesses within the spinal canal, which are openings that allow spinal nerve roots to exit. This narrowing can result from various factors, including degenerative changes, herniated discs, arthritis, or congenital factors. Common symptoms include back pain, leg pain (often in the form of sciatica), numbness, and weakness. Diagnosis involves a comprehensive evaluation, including medical history, physical examination, and imaging studies. Treatment options range from conservative measures such as physical therapy and medications to more invasive procedures like epidural steroid injections or surgery, especially in cases of severe symptoms and failed conservative treatments. Surgical options may include laminectomy and discectomy, depending on the underlying cause of stenosis.