Summary
Piriformis syndrome is a condition that occurs when the piriformis muscle, a small muscle located in the buttocks, becomes tight or spasms and causes entrapment of the sciatic nerve. This can cause pain and discomfort in the buttocks and lower back, as well as numbness, tingling, or weakness in the legs. Treatment for piriformis syndrome typically involves a combination of physical therapy, stretching, and possibly medication to reduce inflammation and pain. In severe cases, surgery may be necessary to release the muscle or to decompress the sciatic nerve.
What is Piriformis Syndrome?
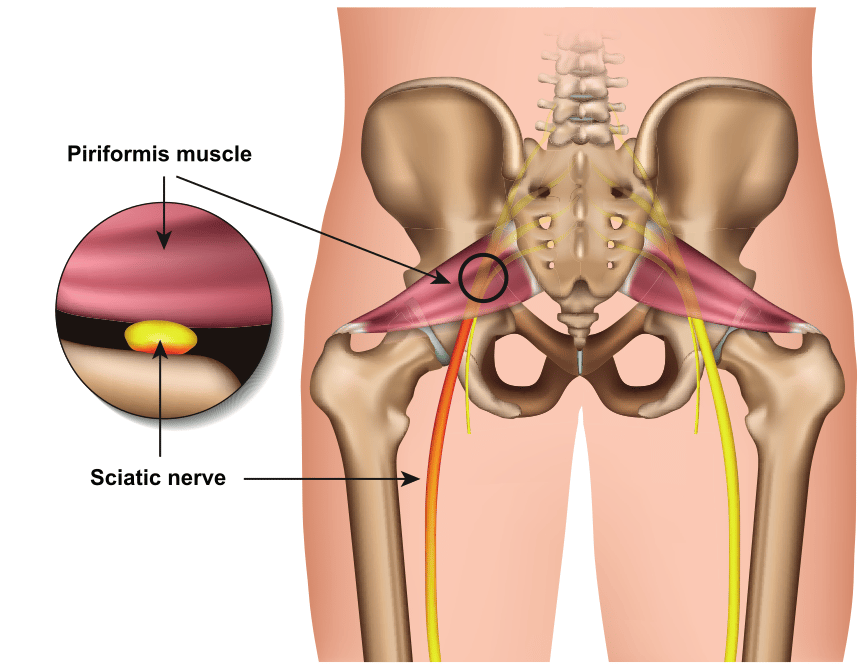
Piriformis syndrome is a painful condition that affects the piriformis muscle, a small muscle located in the buttocks near the top of the hip joint. The piriformis muscle helps to rotate the leg outward and also plays a role in moving the leg backwards and sideways.
Piriformis syndrome occurs when the piriformis muscle becomes tight, inflamed, or spasms. This can lead to entrapment of the sciatic nerve, a long nerve extending from the lower back, through the buttocks, and down the leg to the foot. Compression of the sciatic nerve results in sciatica, a painful condition which may cause pain, numbness, and weakness in the lower back, buttocks, and legs.
Causes
Piriformis syndrome is a painful condition that affects the piriformis muscle and may lead to compression of the sciatic nerve. The exact causes of piriformis syndrome are not fully understood, but a variety of factors may contribute to the development of the condition. Here are a few potential causes of piriformis syndrome, as cited in medical literature:
- Overuse or injury: Repetitive strain or impact activities, such as running or jumping, can lead to overuse or injury of the piriformis muscle, resulting in inflammation, tightness, or spasms.
- Piriformis hypertrophy: In some cases, piriformis syndrome may be caused by a condition called “piriformis hypertrophy,” in which the muscle becomes enlarged due to a genetic predisposition or overuse.
- Anatomical variations: Some people may be more prone to piriformis syndrome due to variations in the anatomy of their piriformis muscle or surrounding structures.
- Stress or tension: Stress or tension in the muscle may contribute to the development of piriformis syndrome.
- Other underlying conditions: Piriformis syndrome may be caused by or related to other underlying conditions, such as sciatica, spinal stenosis, or arthritis.
Symptoms
Piriformis syndrome occurs when the piriformis muscle becomes tight, inflamed, or spasms, leading to pain and discomfort in the buttock area. This can cause compression of the sciatic nerve, resulting in symptoms of sciatica.
The most common symptoms of piriformis syndrome include:
- Pain in the buttocks, especially when sitting or standing for long periods of time
- Pain that radiates down the leg, sometimes resembling the pain of sciatica
- Tightness or spasms in the piriformis muscle
- Tingling or numbness in the leg and foot
- Difficulty moving the leg or foot due to pain or weakness
In some cases, piriformis syndrome may also cause difficulty walking or standing on one leg, as well as a feeling of “foot drop,” in which the foot feels heavy or difficult to lift.
Diagnosis
Piriformis syndrome is often diagnosed through a combination of history, physical examination, and imaging studies.
- Medical history and physical examination: Your healthcare provider will ask about your symptoms, medical history, and any activities or factors that may have contributed to the development of piriformis syndrome. They will also perform a physical examination of your lower back, buttocks, and legs, looking for signs of muscle tightness, spasms, or weakness.
- Imaging tests: Depending on the suspected cause of your symptoms, your healthcare provider may recommend imaging tests such as CT scans or MRI to get a better look at the structures in your lower back and buttocks. These tests can be helpful in identifying inflammation or other changes in the piriformis muscle or surrounding structures.They can help to rule out other conditions, such as a herniated disc or spinal stenosis, that may be causing your symptoms.
- Nerve conduction studies: In some cases, your healthcare provider may recommend nerve conduction studies to assess the function of the sciatic nerve and other nerves in the lower extremities. This test involves placing electrodes on the skin and delivering small electrical impulses to stimulate the nerves.
Treatment
Treatment for piriformis syndrome typically involves a combination of physical therapy, stretching, and exercises to strengthen and stretch the piriformis muscle. In some cases, medications or injections may also be used to help manage pain and inflammation. In severe cases, surgery may be necessary to release the muscle or remove any underlying issues.
Below are specific treatment options that may be used to manage piriformis syndrome:
- Physical therapy: Physical therapy can help to stretch and strengthen the piriformis muscle and surrounding structures, improving flexibility and reducing pain. Physical therapy may also include techniques such as massage, ice or heat therapy, and ultrasound to help reduce inflammation and promote healing.
- Stretching and exercises: Stretching and exercises can help to improve flexibility and mobility in the lower back, buttocks, and legs. Your healthcare provider or physical therapist can recommend specific stretches and exercises to help manage your symptoms.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen may be used to help reduce inflammation and pain. In some cases, your healthcare provider may also prescribe muscle relaxants or other medications to help manage muscle spasms or discomfort.
- Injections: Injections of corticosteroids or other medications may be used to help reduce inflammation and pain in the piriformis muscle.
- Surgery: In severe cases, surgery may be necessary to release the piriformis muscle or remove any underlying issues that are contributing to your symptoms.
The most appropriate treatment for piriformis syndrome will depend on the severity of your symptoms and the underlying cause of your condition.
Sources
Probst, Daniel et al. “Piriformis Syndrome: A Narrative Review of the Anatomy, Diagnosis, and Treatment.” PM & R : the journal of injury, function, and rehabilitation vol. 11 Suppl 1 (2019): S54-S63. doi:10.1002/pmrj.12189
Hicks, Brandon L., et al. “Piriformis Syndrome.” StatPearls, StatPearls Publishing, 4 September 2022.
Vij, Neeraj et al. “Surgical and Non-surgical Treatment Options for Piriformis Syndrome: A Literature Review.” Anesthesiology and pain medicine vol. 11,1 e112825. 2 Feb. 2021, doi:10.5812/aapm.112825