A nerve ablation, also known a neurotomy, is a minimally invasive procedure that uses heat or cold to destroy nerve tissue in order to reduce pain. It is typically used to treat chronic pain conditions such facet joint pain or degenerative disc disease.
There are different types of ablation for the spine, each of which works differently to reduce pain. Two of the most common types include:
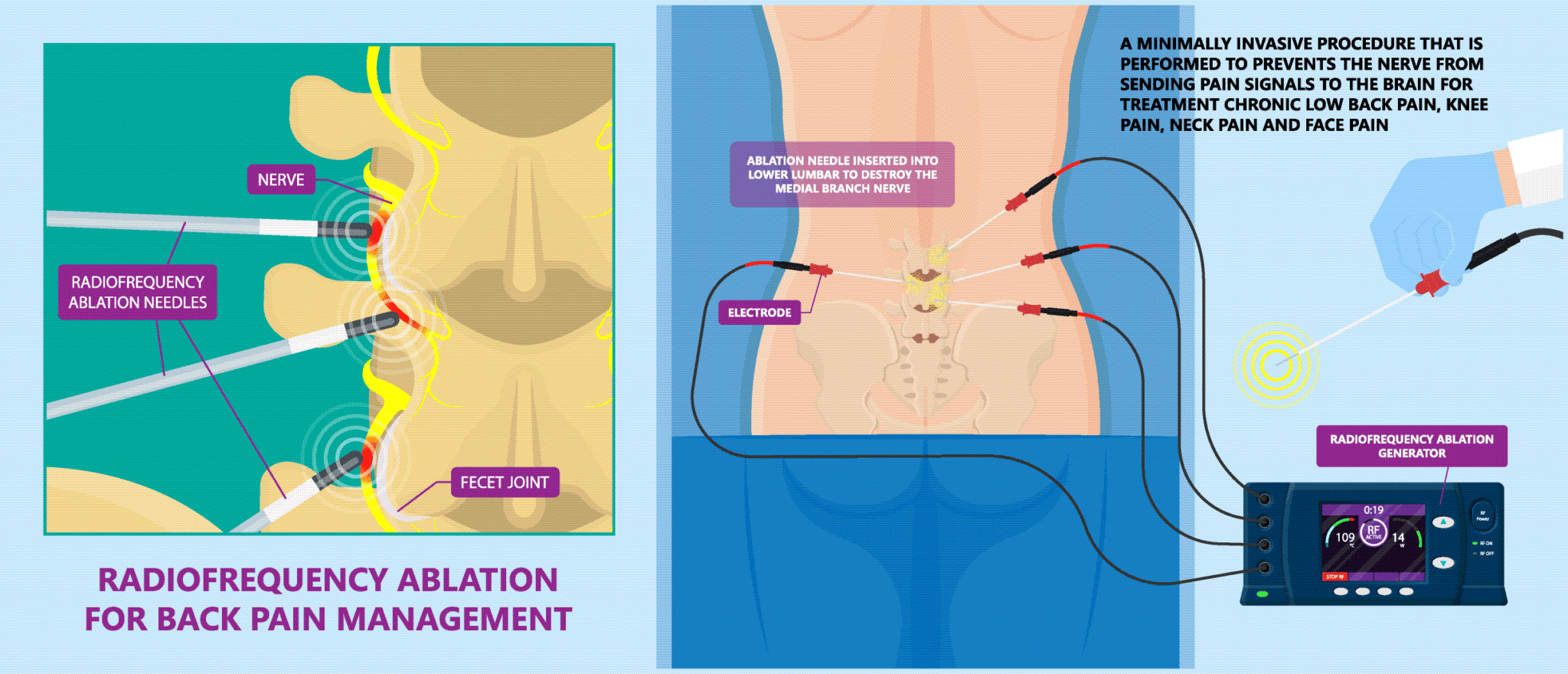
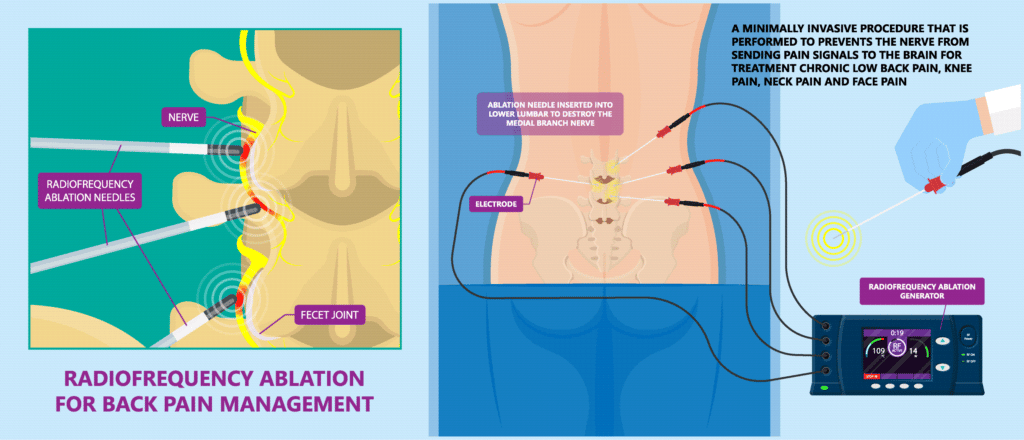
- Radiofrequency ablation (RFA): This procedure uses heat energy to destroy a specific nerve, typically the medial branch nerve, which is responsible for transmitting pain signals from the facet joint. A small needle is inserted into the targeted area, and radiofrequency energy is delivered through the needle, which heats up and destroys the nerve.
- Cryoablation: This procedure uses freezing temperatures to destroy a specific nerve, typically the medial branch nerve. A small probe is inserted into the targeted area, and liquid nitrogen is delivered through the probe, which cools and freezes the nerve.
Which conditions are treated with nerve ablation?
An ablation is typically used to treat chronic pain conditions that have not responded to more conservative treatments such as medications, physical therapy, or other procedures.
Some common indications for ablation include:
- Facet joint pain: Ablation is often used to treat chronic pain caused by arthritis in the facet joints of the spine.
- Spinal stenosis: Ablation is sometimes used to reduce pain caused by the narrowing of the spinal canal.
- Degenerative disc disease: Ablation may be used to reduce pain caused by the deterioration of the discs between the vertebrae.
- Radiculopathy: Ablation is sometimes used to reduce pain caused by a pinched nerve in the spine.
What are the benefits of nerve ablation?
There are several potential benefits of nerve ablation for spine pain, including:
- Reduced pain: Ablation is designed to reduce pain by destroying or reducing the function of specific nerves or tissue that are responsible for transmitting pain signals.
- Minimally invasive: Ablation is typically a minimally invasive procedure that is done under local anesthesia or sedation, which means that it usually involves less pain, bleeding, and recovery time compared to traditional surgical procedures.
- Quick recovery: Ablation is typically a quick procedure, and most patients are able to return to normal activities within a few days of the procedure.
- Long-term pain relief: Ablation can provide long-term pain relief for many patients, which means that patients can get back to normal activities and lead an improved quality of life.
- Cost-effective: Ablation is considered a cost-effective treatment in comparison to long-term medications or surgery.
It’s important to note that every patient is different, and the treatment that works best for one person may not work for another. A consultation with a specialist is important to evaluate the suitability of the procedure for the patient, and to ensure that the patient’s condition is properly diagnosed before proceeding with any ablation.
What to expect the day of procedure
The procedure of ablation depends on the type of ablation being performed and the specific condition being treated. However, the general process is similar for most types of ablation.
- Preparation: The patient will typically be given local anesthesia or sedation to help them relax and minimize discomfort during the procedure. The patient will then be positioned in a way that allows access to the targeted area.
- Insertion of the needle: A small needle is inserted into the targeted area, typically under the guidance of imaging such as x-ray, CT or ultrasound.
- Delivery of energy: Once the needle is in place, the energy, whether it is heat or cold, is delivered through the needle to the targeted area. In case of radiofrequency ablation, a special probe is used to deliver the heat energy to the nerve. In case of cryoablation, liquid nitrogen is delivered through the probe to freeze the nerve.
- Monitoring: The procedure will be monitored with imaging or other monitoring methods to ensure that the correct area is being treated.
- Recovery: After the procedure, the patient will be closely monitored for any complications or side effects. The recovery time depends on the type of ablation performed and the individual case, but most patients are able to return to normal activities within a few days.
What are the risks of a nerve ablation?
Ablation is a minimally invasive procedure that is generally considered safe, but like any procedure, there are some risks and potential complications associated with it. Some of the possible risks and complications include:
- Infection: There is a small risk of infection at the site where the needle is inserted.
- Bleeding: There is a small risk of bleeding at the site where the needle is inserted.
- Injury to surrounding tissue: There is a small risk of injury to surrounding tissue such as the spinal cord or nerve roots.
- Recurrence of pain: The procedure may not be effective in reducing pain, or the pain may return after a period of time.
Is nerve ablation effective?
A 2014 systematic review by Legget, et al. found that radiofrequency ablation results in statistically significant improvement in pain from certain conditions, such as lumbar facet joint and sacroiliac joint pain.
Is a nerve ablation right for me?
Determining whether nerve ablation is right for you will depend on several factors, including the type and severity of your pain, your medical history, and any other medical conditions you may have.
The most important step is to consult a pain management specialist or a specialist in the particular technique you are considering, who can evaluate your case and determine if ablation is a suitable option for you.