If you have ever undergone an MRI, you may have come across a perplexing term – thecal sac indentation (or some variation it). You might have wondered what it means and its significance for your health. In this article, we will delve into the intricacies of thecal sac indentation, exploring its causes, potential implications, and available treatment options. By shedding light on this MRI finding, we aim to provide you with a clear understanding of what it means and it’s significance to your health.
What is Thecal Sac Indentation?
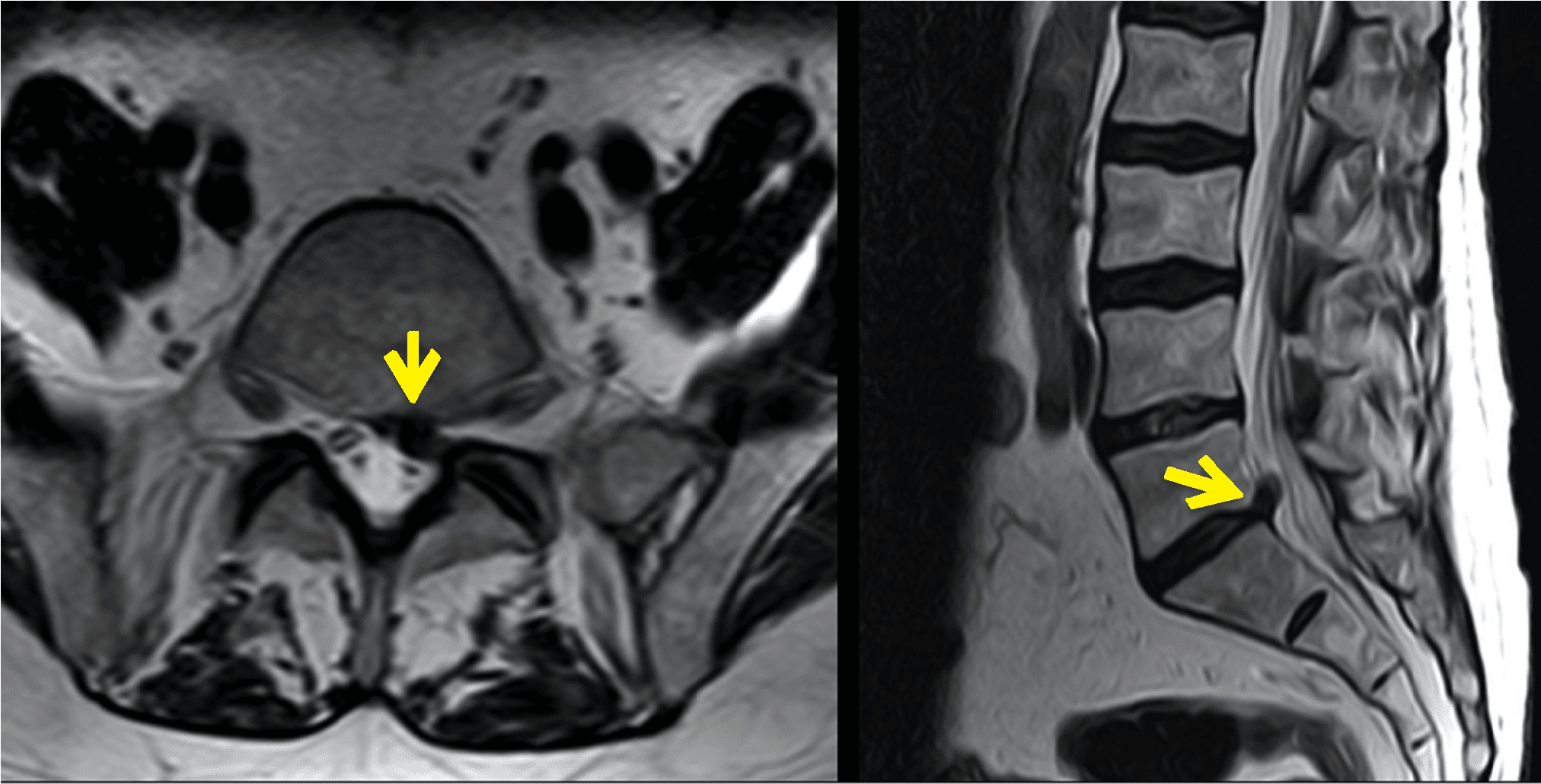
The thecal sac is a protective membrane that encloses the spinal cord and cerebrospinal fluid. It acts as a barrier, safeguarding the delicate spinal cord. Thecal sac indentation occurs when external factors, such as a herniated disc or spinal stenosis, exert pressure on the sac, causing it to become compressed. This finding can be seen on MRI when being evaluated for back pain or other spinal conditions.
Other terms for thecal sac indentation include: effacement of the thecal sac, encroachment of the thecal sac, compression of the thecal
Understanding the Severity
Now, let’s address the question at hand: Is thecal sac indentation a serious condition? The severity of the condition depends on several factors, including the underlying cause and the degree of indentation. In many cases, mild to moderate thecal sac indentation may not lead to significant symptoms or long-term complications. In fact, if the thecal sac itself is being compressed but the spinal cord and nerves are spared, there may be no symptoms at all. However, if the compression is severe, it will effect not just the thecal sac, but the underlying nerves as well. This may lead to painful symptoms requiring medical intervention.
Causes and Symptoms
Thescal sac indentation is often associated with conditions such as disc herniation, spinal arthritis, spinal tumors, and spinal stenosis. These conditions can lead to structural changes or abnormalities in the spine, resulting in pressure on the thecal sac.
Learn more about the causes of thecal sac compression here
If the compression affects not only the thecal sac, but the nerves inside, you may experience symptoms.
The symptoms can vary depending on the location and severity of the indentation. Common symptoms include:
- Back pain: Patients may experience localized or radiating pain in the back.
- Radiculopathy: Compression of nerves can lead to radiating pain, numbness, tingling, or weakness in the legs or arms.
- Neurological deficits: Severe indentation can potentially lead to bladder or bowel dysfunction or even paralysis in rare cases.
If you have any of the symptoms above, it is important to speak to a healthcare professional right away
Treatment Options
Treatment for thecal sac indentation and resultant nerve compression focuses on relieving symptoms and preventing further damage. Non-surgical interventions are usually the first line of treatment and may include:
- Physical therapy: Targeted exercises, stretching, and strengthening can improve spinal stability and alleviate symptoms.
- Pain medication: Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or analgesics may be prescribed to manage pain.
- Epidural steroid injections: These injections deliver corticosteroids directly into the affected area to reduce inflammation and alleviate symptoms.
In cases where conservative treatments are ineffective or if the thecal sac indentation is severe, surgical intervention may be considered. Surgery aims to decompress the spinal cord and nerves, reducing the pressure on the thecal sac.
It is important to note that the decision to undergo surgery is typically reserved for cases where symptoms are debilitating or when there is a risk of permanent nerve damage.
Conclusion
While thecal sac indentation can cause concern, it is not always a serious condition. In fact, if the underlying nerves are not compressed, you may have no symptoms at all. Mild to moderate cases can often be managed with conservative treatments, while severe cases may require surgical intervention. It is crucial to consult with a qualified healthcare professional who can assess your specific condition and guide you through the most appropriate treatment plan.